Newsletter
Published quarterly, this newsletter helps us bring important, interesting, and useful information from the world of medical research and our medical community to our subscribers. Through this newsletter, we illustrate how medical care works through research to make progress in small and large steps.
Each quarter we bring you "A PMH Story": a moment to share how Premium Medical Home has made a difference in the care and experience of our members. Expertise, direct connection, a focus on convenience and optimal practice size promote not only medical care but also the comfort and confidence of PMH members.
PMH STORY
The patient’s daughter called. Her mother had become ill with respiratory symptoms. I went by to visit her at her home. A COVID test was negative. An examination suggested an early or mild pneumonia and antibiotics were prescribed. However, as the afternoon went on, a fever developed and there was weakness, so the member was admitted to the hospital. At the hospital, COVID test was positive, and treatment was started.
Dr. Kelly visited the next day. Visiting a COVID patient, doctor and staff put on PPE - mask, gown, gloves, and face shield. I feel nearly anonymous in PPE. Properly gowned and masked, I went in to see the patient. We had visited often before, so I did not introduce myself. I said good morning, asked if any problems, asked her to lean to the side so I could listen to her lungs. I said, “Deep breath… thank you.” And then listened to her heart and checked for signs of recovery. As I was completing my exam, she said, “Are you Dr. Kelly?” The pattern of my exam, a voice still familiar though muffled by mask and face-shield prompted in her mind the recognition that this was Dr. Kelly, and not one of the many other doctors visiting in the hospital – it is often 5 or more.
It seemed to me that she recognized, behind layers of PPE, that this was someone she knew. I think this does good for the patient’s confidence and recovery. It was a reminder of how unrecognizable we are behind COVID personal protective equipment and how there is a benefit to seeing our doctor, our personal doctor in the hospital.
Robert H. Kelly, MD FACP
PMH STORY
“Thank you for seeing me today.” It is a common greeting in our PMH practice, where we have a commitment to being “not too busy.” The patient had called because she felt lightheaded after several days of a mild cough. We asked her to come to the office right away. We discovered infection with COVID and low blood pressure. The blood pressure responded well to oral hydration and the COVID infection was treated with antivirals. By the next day, the patient was feeling better and went on to an excellent recovery.
Increasingly, we recognize how difficult it is for people to see their own doctor for a same-day appointment. The president of the American College of Physicians, Isaac Opole, wrote a detailed essay this December 2024. He talks about a friend of his who “described in horrific detail how she almost lost her life,” because she could not make an appointment with any of her doctors. Though an internal medicine specialist herself, she was unsure of the meaning of her symptoms and was told that there was no available appointment with any of her doctors. The next day, feeling worse, she went to an emergency room, where she was found to have significant anemia along with congestive heart failure. Dr. Opole goes on to say, “the primary care machine is slowly, but certainly grinding to a halt. The doctor cannot see you now.” At PMH, we believe an internal medicine office should be run in such a fashion that the doctor can see you today. We plan to be able to say to patients who are ill and who would benefit from the same-day appointment that they can come to our office where the nurses and the doctor know them well and will welcome them. We believe this makes medical care better.
Dr. Opole and others are perplexed by how to improve availability of internal medicine care in a timely way. This is a problem that we have faced as well and our decision to embark on the PMH effort was motivated in part by the need to provide care in a timely and accessible way. We will continue our efforts in this regard. We hope that you will discover that if you need us, we are not too busy.
We know that emergencies can arise, and we may need to use urgent care or an emergency room. But our goal is to make this office available to you when you need it.
Allan R. Kelly, MD FACP
PMH STORY
A fine internal medicine doctor called to discuss a County Medical society issue with Dr. Kelly. She has had her own internal medicine practice in Tarrant County for decades and increasingly feels challenged and not sure what is going to happen with her practice. She feels like the world of internal medicine is closing. That is not why she called the office, but it is what she reflected on as she listened to the message on Dr. Kelly’s answering machine. She called around 5:00 on a Saturday, and she listened to the message, in my own voice, where I say, “If you did not get an answer at the office, please call my cell phone, 817-360-0408.” The cell phone was repeated, and the answering service number was given.
The internal medicine doctor told me that as she listened to the message, she was “dumbstruck.” She sat silent and tried to come to grips with what she had just heard. She heard a doctor share his cell phone number with any patient or family member who needed to talk to him. She heard a doctor who wanted to help a patient or a family who might have questions or concerns when the office is closed. She did not hear the phrases she is so familiar with: “If this is an emergency, hang up and call 911” or a long description of the office hours and telling people to call their pharmacy first and other instructions that we have become accustomed to. She called back and listened again, writing down the cell phone, and called me about the medical society issue.
She told me that she felt energized just to hear my message. She told me, “That is what I would like to do.” I encouraged her to think about it and let me know if I could help. We finished our business, and she said goodbye. This was my first time ever to actually talk to this colleague. Her reaction illustrates what we are doing here at Premium Medical Home. How do we make medical practice good and even beautiful to patients, families, and the doctor? How do we do a really good job so that our colleagues and our families can benefit?
We experience PMH stories every day. Direct contact, not too busy, professionalism, continuity of care, and affordability are amongst the many goals we set for our practices. We will continue to strive for those goals and to serve our patients and their families and our community as best we can.
Allan R. Kelly, MD FACP
DO “STRONGER” PAIN MEDICATIONS BEAT OVER-THE-COUNTER MEDICINES FOR PAIN RELIEF AND ARTHRITIS?
Over the past several years, there have been a number of randomized controlled trials looking at the effect of narcotics on osteoarthritic pain. A review of these trials appeared in “ARTHRITIS CARE AND RESEARCH.” It studied the effect of a narcotic, tramadol. Tramadol is reasonable and can be used with a doctor’s prescription. We used to look upon tramadol as a way of increasing pain relief options for our patients if over-the-counter medications were inadequate. We used to think that if the patient with osteoarthritis asked for “something stronger for my pain,” then a narcotic was the answer. This is likely not true. In this review of randomized controlled trials, there was no difference in pain relief with the narcotic medication tramadol, compared with over-the-counter medications. However, the incidence of adverse events was considerably higher with tramadol. Looking specifically at problems of osteoarthritis, randomized controlled trials do not show that narcotics give better pain relief for chronic osteoarthritic pain compared to over-the-counter meds. The presence of significant adverse events makes the narcotic unadvisable.
There are situations where acute pain syndromes, such as after an operation, benefit from the use of narcotic therapy. But for chronic pain disorders, the role of narcotics is growing smaller and smaller.
Allan R. Kelly, MD FACP
INDIGESTION
Indigestion is a common problem. It reflects the normal action of the body causing symptoms. It is characterized by symptoms such as feeling too full after a meal, having a decreased appetite, epigastric burning/discomfort, and present on a weekly basis for months. Symptoms should be reported if they are new, increasing in severity, or causing any alarm signs such as diarrhea, vomiting, fever, or signs of blood.
There are many options, both prescription and over the counter, help relieve functional dyspepsia or indigestion. First, Prilosec and famotidine can be helpful and should have an early role in self-care. Research studies have also looked at peppermint, caraway, turmeric, and Iberogast. Iberogast is a combination herbal formulation for IBS and bloating symptoms. Randomized studies have shown a 20% to 50% improvement in symptoms, not perfect answers, but for some, maybe a helpful remedy. Call or visit if symptoms trouble you.
Robert H. Kelly, MD FACP
SOCIAL MEDIA AND HEALTH
Research published in JAMA Pediatrics this year shows that there is harm from heavy use of social media. A metanalysis of 126 studies of social media use in teenagers demonstrated that frequent versus infrequent social media use was associated with increased alcohol consumption, drug use, tobacco use, sexual risk behaviors, and gambling. Cause and effect are not established, but the association causes worry. American Heart Association in 2013 documented an association with obesity. In 2023 the Surgeon General issued a report of the harmful effect of social media use on young people. American Journal of Psychiatry published a study in adolescents – 30 minutes social media use in adolescents correlated with reduced coping skills that became more severe as social media use increased to 180 minutes daily. Pediatric societies in the United States and the UK and the World Health Organization have developed guidelines on safe screen use, including limiting use, age-appropriate content, and discouraging isolation with the tablet. It appears that high early life digital media exposure can affect intellectual and psychosocial development in children. Average tablet/mobile device use in2020 was 5 minutes increasing to 55 minutes in 2022. A study in 2024 studied use(30minutes) at age 3.5 years and identified 22% increase in anger and frustration after one year of such tablet use by 3 1/2-year-olds.
Perhaps social media on tablets, phones, and computers distract attention from the real work of life. Conversations with our family, engagement in a community, skill development, time spent in ordinary play has potential for healthy coping and growth that entertainment does not have. We encourage adults and children to be alert to the adverse effects of social media.
Robert H. Kelly, MD FACP
QUOTES
It is no longer a secret that for many Americans it is …almost impossible to get a primary care appointment for a routine care in a reasonable amount of time.
Isaac Opole, MD, President, American College of Physicians, 2025
It is important to acknowledge that medicine is not just about procedures and tests, but also time, connecting with and listening to our patients. After decades of research, I think there are three traits that are essential for any physician: Listening to patients, humility, and curiosity.
Hardeep Singh, MD, 2024
I doubt that charting, coding, and billing are on the patient’s or the family’s mind.
Rachel Fleishman, MD, 2024
Being more active and eating better are associated with better surgical outcomes…I was surprised at the size of the benefits.
Daniel M. Isaac, MD, 2025
I am inspired by and grateful for the people who help, who bend rules to arrange an admission, or break rules to let a spouse shower in a hospital room. We need more of this, and I wish we needed none of it at all.
Heather Kovich, M.D., 2024
Life affords no greater responsibility, no greater privilege, then the raising of the next generation.
C Everette Koop, MD 1985
At its foundation, medicine is constituted by a particular kind of relationship, one based upon trust between a patient made vulnerable by illness and a doctor who professes to use his knowledge and skills always and only for the purpose of health and healing.
Aaron Kheriaty 2024
I admonish physicians, above all other considerations, to be honest. I mean honesty in every conception of the word: let it enter into all the details of your work.
William Mayo MD 1910
The object of all health education is to change the conduct of individual men, women, and children by teaching them to care for their bodies well.
Charles Mayo, 1932
PMH STORY
The patient was a hospital administrator with decades of experience. She was familiar with physicians, hospitals, and outpatient clinics. She had medical problems and required the care of her internal medicine doctor and her consultants. This is a story about how doctors’ offices answer their phones.
Her cardiologist had cared for her for over a decade. She came to the PMH office for a follow-up appointment and mentioned that she has had to change her cardiology doctor. She said that whenever she tried to talk to the doctor or to call the doctor’s nurse, she always had to go through a long, computerized message, then various choices, and number pressing. In the end, she would leave a message. She did not know who would get the message. Increasingly, she had noticed that the messages seemed not to be acted on or returned. All she wanted to do was change an appointment time. Even though sophisticated in medical matters, she could not understand the website, the instructions, or the voice messages to successfully change her appointment. She changed to another cardiology office where the phones were answered more quickly, though still with a long series of messages. It was better. She remarked that the computerized answering machines and such seemed to be an unavoidable barrier to Care.
At our PMH office, we also run into this: when calling doctor’s offices or hospitals where it is difficult to get through to a person. We are aware of how hard this can be on our patients and their families. We continue to use an employee answering the phone promptly with human voice, human resources, and human ingenuity to address the questions, problems, or concerns of our patients, families, or colleagues who need help from our office. We believe this type of answering is helpful and meaningful to patients and other people who need our office to help them. It does add to the “work” as phones must be monitored and answered. It is one important way doctors serve their community: by answering the phone quickly and responding intelligently, thoughtfully, and promptly even if it is simply to change an appointment.
For many of our younger patients, online access to making appointments or dealing with problems is outstanding, but that does not work for everyone, and it is the frailest and the elderly who need direct, personal attention the most. Also, people who are sick, in trouble, or facing an emergency are helped the most by a quick human answer to their call.
PMH helps patients and families.
Allan R. Kelly, MD FACP
CRANBERRY AND UTIs
A recent review was published in an online medical journal about cranberry tablets in reducing the risk of UTIs. Overall, there was a 27% reduction in the risk of UTIs in those using cranberry juice or cranberry juice capsules compared to placebo. There is a greater benefit with the juice compared to the capsules, possibly because of the extra water with the juice (i.e. hydration). Nevertheless, both reduce the frequency of UTIs. Other research shows that mannose, a carbohydrate supplement excreted in urine, adds to the preventive effects of cranberry. Together, mannose and cranberry are over the counter supplements that protect people from recurring bladder infection.
Robert H. Kelly, MD FACP
STATINS AFTER AGE 85
Guidelines in the past 20 years have not included statin therapy in people over the age of 85. We know that in older adults with cardiovascular disease statins are prudent, helpful, and meaningful. But how about adults over 85 with no history of cardiovascular disease? Researchers at University of Hong Kong did a trial, (Annals of Internal Medicine in May 2024), where initiators and non-initiators of statin therapy were closely matched and compared using statistical and medical comparisons. They were not randomized. Researchers showed that the value of statins in reducing health risks was greater in the over 85-year-old patients than the value in the 75 to 85 and in the under 75 population. All-cause mortality was reduced by 10 to 20%, more in the over 85 group compared to mortality risk reduction in the under 85 group.
The number of lives saved shows the value in the over 85. Specifically, the number of events was reduced by 12% in the over 85 group over a period of five years: from 39% death rate in the non-treated group and 26% death rate in the treated group. The incidence of adverse drug effects in the treated and untreated groups was the same – there was no reported increased risk of adverse effects in the statin treated Group.
This study calls into question the recommendations of the American College of Cardiology and the United States Preventative Services Task Force. I hope to see randomized controlled trials with older Americans soon. We hesitate to use words like cause and effect when it is not a randomized controlled trial. There is a movement afoot in some large journals, such as the New England Journal of Medicine, to allow researchers and doctors to use cause and effect language derived from observational trials. The authors in this Annals of Internal Medicine article do not indulge in cause- and-effect language. They prudently comment that this is what they observed.
Allan R. Kelly, MD FACP
SWEETS AND HEALTH
The Nurse’s Health Study recruited over 30,000 volunteers from 1984 to 2016 to study health outcomes related to individual choices. Research reported in 2024 showed there was a trend of increased autoimmune disorders, especially lupus, related to ultra- processed foods. Higher cumulative average daily intake of ultra-processed food was associated with a 56% increase in the incidence of lupus, especially lupus with anti- double stranded DNA antibody. Artificially sweetened beverages, and even sugar use, were also associated with autoimmune disorders. Body mass index, on the other hand, had no relation.
Avoiding ultra-processed food, concentrated sweets, and artificial sweeteners is good advice. There is the association with specific disease processes. In this example, an autoimmune disorder called lupus. For your better health, it is best to minimize ultra- processed and sweetened foods. Both natural and artificial sweeteners increase health Risks.
Robert H. Kelly, MD FACP
VITAMIN K AND MUSCLE CRAMPS
Muscle cramps are common, painful, disruptive, and generally not dangerous. In the past, quinine was used by our parents and grandparents; but now, quinine is seen as a potentially dangerous drug. Over-the-counter quinine has been removed from the market. Some muscle cramps are related to serious medical problems, such as atherosclerosis, inflammatory myositis, electrolyte disturbances, and serious motor neuron, and spinal cord disease. But these serious issues are uncommon. Most nocturnal muscle cramps are benign and idiosyncratic.
We know that exercise can reduce the frequency of cramps. Even a 5-to-10-minute walk before going to bed can make a big difference. But people are also interested in medication they might take at bedtime to help. Supplements like magnesium, potassium, or calcium are commonly used.
But persuasive data from randomized controlled trials supporting supplements is limited. That is why a report in JAMA Internal Medicine is important. Researchers in China, reported a randomized controlled trial in healthy adults over the age of 65 years. In this trial, participants with severe nocturnal muscle cramps received a vitamin K2 supplement or placebo. The K2 was 180 mcg, and is specifically menaquinone-7, abbreviated as MK-7 on bottles of these supplements. The participants were interviewed weekly to report on the incidence of muscle cramps that interfere with sleep. At baseline, the participants reported approximately 2.6 painful cramps per week. At the end of eight weeks, the placebo group was experiencing on average 3.63 painful cramps weekly. The vitamin K group was experiencing 0.96 painful cramps per week. The reduction in the number of cramps from approximately three weekly to less than one weekly is significant.
In summary, a randomized controlled trial, performed in China, showed convincing evidence that a Vitamin K3 can reduce the frequency of leg cramps in healthy individuals. I expect there will be other groups trying to confirm this information.
Allan R. Kelly, MD FACP
ZINC FOR COVID
In 2023, Abdallah, et al., reported results of an experiment where people with covid were randomized to placebo or zinc tablets. After diagnosis with a PCR test, patients were randomized to oral elemental zinc (25mg daily) or matching placebo. The patients were compared regarding duration of symptoms and adverse outcomes such as hospital admission and death. The mean age was 54 years. Poor outcome was 17% in the placebo group and 10% in the zinc group. There was no difference in the death rate between the two groups. The patients treated with zinc had milder symptoms by the 15 th day of their illness, and symptoms resolved sooner. Paxlovid and molnupiravir are effective treatments for covid illness but are also potentially very expensive and may cause side effects. Now we know that inexpensive, non-prescription zinc tablets also help people with a covid infection.
Robert H. Kelly, MD FACP
QUOTES
If we could give every individual the right amount of nourishment and exercise, not too little and not too much, we would have found the safest way to health.
Hippocrates, 301 BC
No greater opportunity or obligation can fall to the lot of a human being than to be a physician. In the care of the suffering, she needs technical skill, scientific knowledge, and human understanding.
Tinsley Harrison, M.D. 1950
Instead, take these patients’ preferences seriously as a way to respect them aspersons and to protect their liberty. Physicians’ reluctance to treat patients over theirobjections may therefore reflect a well-founded moral intuition rather than mere self-interest or pragmatism.
Mark Navin, Ph.D. 2019
You survive in the new [medical care] system by giving the computer complete attention, the kind of attention we used to reserve for a patient. By default, the patient moves down to second place. As sad and horrifying as this sounds and feels, it is becoming the new reality.
Elizabeth Toll, M.D. 2020
If we are not careful, we might even convince society that the electronic medical record, and what it represents, is an end in itself, more important than taking care of the sick, training or successors, and finding cures for human disease. Or is it already too late? Has the door already closed behind us?
Martin Samuels, M.D. 2022
At its foundation, medicine is constituted by a particular kind of relationship, one based upon trust between a patient made vulnerable by illness and a doctor who professes to use his knowledge and skills always and only for the purpose of health and healing.
Aaron Kheriaty, M.D. 2024
Even though many physicians have traded the traditional shingle on the door for the big health system billboard, the obligation to provide the best care possible for each individual patient remains, physicians must continue to take personal ownership of every interaction with their patients. We must remember that despite the beautiful waterfall in the lobby and the self-playing piano in the cafeteria, the patient walks in the door seeking care from us, the physician, not from the system.
Isaac Opole, MD, 2024
PMH STORY
The niece was managing her aunt’s affairs while she was living in another state. She asked me if I could take care of her aunt, and I agreed. I cared for her for 7 years after she moved into a care center. She suffered from severe dementia. Her health was otherwise good. She rarely left her room. Over time she remained in bed.
From our first visits, she was reluctant to see me. She was unwilling to see any doctor. Nurses were told to leave her alone. Most of my visits ended with her saying “go away” or “please leave now.” I visited briefly to make sure she was OK. Her goal of care was to be left alone, but in a care facility especially, a patient cannot be ignored. I understood her instructions and respected them.
She became ill with Covid. Staff called me. Her temperature was elevated, 101 o . The bedside test was positive. I ordered Paxlovid. Two days after the onset of symptoms, I went by to see her. Her room was neat and orderly thanks to the good staff at the facility. She had her TV on. The blinds were up on the window. She was in bed, and she seemed like her usual self. She was mildly ill There was slight congestion, and staff reported some coughing.
I let her know that I was Dr. Kelly, that she had been ill, and that I was there to check on her. I listened to confirm that there was no Covid pneumonia. Her examination was stable and safe. I told her the illness was caused by Covid, and that she was doing Well.
She then said more to me than she said before. She said, “Is everybody getting this?” I told her that Covid was getting to be common again but fortunately was not causing much harm, just a troubling viral infection. I asked if there was anything else her doctor could do for her. She said no. I straightened up to leave. She said to me, “Thank you for taking care of me, Dr. Kelly.”
At PMH, we think there is more to a doctor visit than checking off boxes on a sheet or computer. Visits are based on shared goals, expertise, knowledge, and experience. For her, our visit confirmed her illness with Covid and her effective treatment. It is both a PMH story and a story for doctors. You see your patients. You take care of them. You do right by them. Even if the words are unsaid, we trust they will be able to say silently or out loud, “thank you for taking care of me.”
Robert H. Kelly, MD FACP
INSOMNIA
Insomnia troubles most of us at some point in our lives, hopefully just for a day or two at odd times. But it can be a chronic condition. It is hard to say with confidence how many hours a person should sleep or what normal sleep is for each and every person. What we all desire is to feel rested when we wake in the morning. Key options to treat insomnia are cognitive therapy, sleep hygiene, sleep restriction, and stimulus control. Cognitive therapy involves changing false beliefs and attitudes about sleep, for example, the idea that one needs 8 hours of sleep, and not committing to some artificial doctrine such as “I need 8 hours of sleep”. What you need is sleep so that when you get up and go in the morning and you feel that you have rested.
Improving sleep hygiene includes abstaining from alcohol, using no caffeine or nicotine after 4pm, avoiding exercise within 2-4 hours of bedtime, going to bed and getting up at consistent times, not watching the clock when you are trying to sleep, reducing nap time during the day, and not watching television or using electronic devices in bed.
Sleep restriction is perhaps best accomplished by setting a clock to get up out of bed at a time that is proper for you and making this standard every day. This is individual, but looking back over the weeks and years, most of us know that we are best when we get out of bed by a certain time. Getting up at a consistent time everyday becomes the principal element of time restriction. If you are spending time in bed unable to sleep, then the amount of time you spend in bed should be restricted.
Finally, stimulus control is important to getting good sleep. If unable to sleep, it does not hurt to get up out of bed and go to another room. Keep the bed for sleep and not for worry, reading, or electronic entertainment. If you are not sleepy, then finish what you are doing, go on to another task, and go to bed when you are sleepy.
Robert H. Kelly, MD FACP
IRRITABLE BOWEL SYNDROME: OLD DRUGS, NEW TREATMENT
Irritable bowel syndrome (IBS) includes abdominal pain and discomfort before or after bowel movements that are disruptive or difficult for patients.
New research in The Lancet studied an old drug, Elavil. It was first approved for use in United States in 1961, 63 years ago, for depression, insomnia, and chronic pain. 463 patients with irritable bowel syndrome were randomized to placebo or Elavil. Elavil was prescribed in low doses, starting at 10mg. The use of Elavil increased the rate of resolving IBS by more than 50% compared to placebo. The risk of discontinuation due to side effects was greater in the placebo group than in the Elavil group. The study shows how there can be beneficial uses of old drugs that have not been explored. Old drugs tend to be inexpensive, and the risk and benefits are well known. Such use is considered off-label by the FDA, but it is not off target.
Allan R. Kelly, MD FACP
LOWER BACK PAIN: HOW TO PREVENT A RECURRENCE
Researchers from Australia published results of a randomized controlled trial in Lancet this year. They randomized 351 adults to routine lower back pain care or routine lower back care plus an intervention. The intervention consisted of six sessions of progressive walking with a physical therapist. The sessions occurred once a month for six months and emphasized walking at home to help with the back pain. The mean age of the participants was 54 years. The primary outcome was the number of days to recurrence of lower back pain severe enough to limit activity.
Time that passed before the person suffered serious back pain recurrence took 112 days in the control group and 208 days in the walking group. In the control group, twice as many people sought medical care for their back as in the walking group. Walking therapy markedly improved back pain outcomes.
This simple experiment showed that getting up and walking at least once a month and encouraging walking at home made a big improvement in back pain. One way to interpret this insight: encourage people with a bad back to get up and go for a walk. Walking can help relieve pain.
Allan R. Kelly, MD FACP
OVER-THE-COUNTER BIRTH CONTROL PILLS
We have previously discussed how making medical care directly available to people without requiring a doctor’s order can improve health. Whether UTI, Covid, or pregnancy, there is great value in putting reliable diagnostic tests in personal control. We have known for decades that safe medicines available to individuals can prevent medical problems, like peptic ulcers and sunburn.
Since March, oral hormonal birth control pills are available without a prescription. The product is made by Perrigo Company and is marketed as “Opill.” The cost is approximately $20 per month. The medication is a progesterone only birth control pill approved by the American College of Obstetrics and Gynecology.
The opening up of medical care to personal choice, not restricted to those with a license, will improve people’s access to care. Allowing individuals to make a personal decision about what they want and what they think is best likely improves well-being. There will be isolated stories of tragedy that will be blamed on the easy availability of this product. Time will tell where this liberation goes.
Allan R. Kelly, MD FACP
REPLACING AORTIC VALVES: AN EASIER WAY
Technology is fascinating. A life-changing, society-changing technology, like heart bypass, will itself become a target of innovation. This is as true in medicine and surgery as it is in, for example, the world of computers and automobiles.
Dr. Michael DeBakey and others introduced valve replacement surgery. It changed the world. These first artificial valves required cardiac bypass machines, a large surgical incision, multiple transfusions, and heroes like DeBakey and Cooley. Artificial valves have saved untold lives.
In the 1990s, doctors began to innovate. The new artificial valve could be introduced through a small incision in an artery and then transported via catheter to the aortic valve and expanded in the place of the native valve.
In the New England Journal of Medicine in May of 2024, researchers looking at patients with moderate to severe aortic valve stenosis randomized patients equally to open heart surgery, or transarterial catheter technique. Initial results of this randomized control trial are important: The likelihood of death from any cause was reduced by more than 50% in the transcatheter valve replacement. The likelihood of stroke was reduced by approximately 40% in the transcatheter patient compared to the surgical intervention. This is a short-term follow-up, only one year. Five-year follow-up or 10-year follow-ups are planned and could change the apparent value of the transcatheter technique.
It is wonderful to see progress and innovation in medicine and surgery in our world today. We all benefit from the insight, innovation, and experimentation created by prosperity, education, and encouragement of opportunity. We create a better world by encouraging our surgical and medical colleagues (and ourselves) to come up with better ways, better techniques, better care.
Allan R. Kelly, MD FACP
SWEETENERS: REDUCE!
It seems right when international guidelines seem to correlate with common sense. Recent WHO guidelines about artificial sweeteners seem like common sense. The focus was on obesity, body weight, and the incidence of diabetes. They find that there is no health advantage to using artificial sweeteners, especially in those who are seeking weight loss or who have diabetes. The WHO data showed that higher use of non-sugar sweeteners was associated with increased diabetes.
The WHO concluded that people should reduce sweetness in their diet altogether, starting early in life in order to improve health. That is common sense. Sweet foods are good for dessert or for treats but should not be a part of our daily or usual diet.
Reducing the use of sweeteners, sugar or artificial, is a worthwhile health goal. Artificial and sugary beverages should be avoided.
Robert H. Kelly, MD FACP
QUOTES
Technology is separating us from patients. 2500 years ago, Hippocrates wrote that “some patients, though conscious that their condition is perilous, recover their health simply through their contentment with the goodness of the physician.”
Salvatore Mangione, M.D. 2024
“It’s brutal,” a patient told me. She was not talking about her COPD, but the loss of her third primary care physician in two years. This churn in practitioners is not examined nor benchmarked.
Walter O’Donnell, M.D. 2024
A better name for the general practitioner might be multispecialist.
Martin Fischer, M.D. 2008
Every surgeon carries within himself a small cemetery, where from time to time he goes to pray – a place of bitterness and regret, where he must look for an explanation for his failures.
Marsh, M.D. 2024
PMH STORY
Sunday morning I went to the emergency room to meet a patient. This ER has more than 100 beds, and hallways are frequently used as well. As I walked to my patient’s room, I noted that 4 of the 20 people in hallway beds seemed healthy, looking well. I have learned over the last 10 years that they were here because they did not have a place to get medical information or to see a doctor other than in the emergency room. Sitting at the physician’s desk, I could see and overhear one of these younger couples. The man, wearing jeans and boots, around 35yo, reclined on an ER stretcher, his wife at his side. The clerk was going over the paperwork and told the patient that the estimated cost for the visit would be $7,347. The wife exclaimed, “$7,000!”
Several weeks later, a patient called me on a Saturday morning. There had been an operation several days earlier, and it took many attempts to get the IV in place before surgery. That day, he went home with good operative outcome. But the area where many nurses had tried to draw blood and start an IV was very sore. I asked him to come to the office to check this. Examination was favorable; advice and information was given. As the patient left the estimated cost would have been $50, for an office evaluation, not thousands of dollars.
PMH provides multiple benefits to physician and patients. For patients, it provides continuity of care, direct relationship with physicians, respect for the patient’s convenience, and a practice that is not too busy. One example is being able to call a doctor and ask if something is likely important or not. And you’re not talking to a stranger, but to a doctor that knows you, has seen you and spent time thinking about your care and your health. You’re able to see a doctor at short notice, to visit in person with a physician whether online, at the office, or in your home. I realized that not only does this serve the personal needs of the patients, but it reduces the times you may find yourself in the ER being told that the estimated cost to get an answer to your question is $7,000. A non-PMH model of care may be more expensive and less convenient. There is a charge for PMH, but we think it can be a way to save money.
Robert H. Kelly, MD FACP
GLP-1 DRUGS (LIKE OZEMPIC) VERSUS INSULIN
Sometimes diabetes is not easily controlled. All patients are encouraged to lose weight, to exercise, and to follow a diabetic safe diet. Ozempic and Mounjaro are the semaglutides (peptides) used to treat diabetes and obesity. A recent experiment compared Mounjaro to as-needed insulin in patients suffering with diabetes and already on once daily long-acting insulin. In years past, with the failure of such treatment, they would almost certainly be started on mealtime insulin, requiring one, two-, or three-times daily finger stick sugar measurements. Replacing 10 to 20 weekly injections of insulin and 10 to 20 weekly measurements of sugar with a once weekly injection of a peptide t would be a huge advance for patients.
In the experiment reported by researchers in Dallas and Spain, adults, average age 58, with poor control of diabetes despite long-acting insulin, were randomized either to Mounjaro once weekly or taking short-acting insulin three times daily. (With all volunteers continuing once daily long-acting insulin.) Mounjaro was significantly better than with insulin as far as improvement in diabetes control. Hemoglobin A1c improved dramatically in the Mounjaro group compared to the short acting insulin group. Worse for insulin, the short-acting insulin group suffered greatly from intermittent low sugars. Severe hypoglycemia occurred in 4% of the insulin-treated group and in none of the Mounjaro-treated group, and severe hypoglycemia is dangerous and can be deadly.
The complications of insulin therapy were prevented by using Mounjaro instead of short- acting insulin. There was nausea in some of the Mounjaro group. More serious adverse events did not differ. GLP-1 drugs, like Ozempic and Mounjaro, are better than what we have been doing before. Improving the care of diabetics, we believe, and expect, will save lives, prevent complications, and improve quality of life. The new drugs are better than insulin, according to this randomized controlled trial. This is a revolution in medical care.
Allan R. Kelly, MD FACP
HOME TESTING
Relaxing regulations gives people more options, improves care, and increases what people can do for themselves. High standards are important, but regulation limits who can provide care and the circumstances of care.
Over-the-counter self-testing kits continue to be an outstanding example of how deregulation improves care. The availability of over-the-counter pregnancy tests has changed the lives of many people. Then there is the ability to check urine for infection, to check sugars for diabetes The COVID emergency led to deregulation of viral testing at home. Having COVID testing at home improved care.
In January 2024, Pfizer began offering an at-home test for influenza A, influenza B, and COVID. But this test offers another breakthrough: it uses PCR testing, which is significantly better than the prior rapid antigen test. There was a battle to get this approved and deregulated so that Pfizer could offer something better to the public. It is too early to make any general statement. I am excited by the possibility of improving people’s ability to care for themselves, with or without the advice of a doctor, at home. And for people to learn if they or a family member has flu or COVID, improves the ability to protect health and save time and money in a prudent, reasonable, and loving way.
Congratulations to Pfizer Corporation. Thank you to the bureaucrats who allowed Pfizer to bring this product to market. And our deepest appreciation to those over the decades who have tried to bring better medical care into the homes of all of our patients.
Allan R. Kelly, MD FACP
PMH: CREATING AN ALTERNATIVE TO SHALLOWNESS
A mystery in the world of medicine today is the growing attention to physician “burnout.” We see it in our journals on a weekly basis. David Vermette, MD, in JAMA, April 23, 2024, is an example: “Burnout is rampant, imposter syndrome is endemic, and fatigue is the norm... [for physicians today]. Disillusionment with the practice of medicine can begin during medical school and often amplifies during residency. How does one reconcile their lived experience of being a physician with the ideals they envisioned when they first embarked on the journey?”
In our decision to embark on the PMH project, we wanted not only to create a medical practice that the patient and the patient’s family thought of as “better,” but also to create a work environment and a practice that would appeal to the doctors and nurses who work in our clinic. We have focused on this from the beginning. In part, we were responding to the increasing risks that medical practice was headed in the direction described by Dr. Vermette. We will continue our efforts to create a practice where burnout and its associated symptoms do not occur. We bring multiple medical students into our office every year to show them a possible future for themselves and their colleagues. We appreciate the support of our patients and patient’s families, as well as our colleagues, as we keep developing.
Allan R. Kelly, MD FACP
THYROID DOSE IS IMPORTANT
Persons with low thyroid are treated with thyroid hormone, either synthetic (levothyroxine) or natural (Nature-Throid, Armour Thyroid or thyroid hormone). As there is a narrow therapeutic index or margin between safe and not safe, monitoring is done to make sure the dose is correct. Dosing accuracy is determined based on hormone levels measured in the blood, either pituitary hormone TSH or levels of actual thyroid hormone (T3 or T4) in the blood, repeated approximately every 6-12 months. A study was done to look at the risk of dementia with excessive thyroid hormone treatment. The study populations were persons over the age of 75 years. The degree of excess thyroid hormone was either moderate or severe. The risk of dementia, all measured over the course of approximately up to nine years, was 50% to 60% higher in the severely overtreated group.
Even if you are feeling well on your current dose of thyroid hormone, it should be checked about every 6-12 months. If lab tests show excess replacement, then the dose should be reduced. Correct dose is not based on your own personal perception of treatment effect, though that is important to discuss. Accurate dosing is based on measurement of the levels of pituitary and thyroid hormone. The goal is for the hormone levels to be normal on treatment. Doctors love normal.
Robert H. Kelly, MD FACP
ORDINARY SUPPLEMENTS FALTER IN STUDY
Some common supplements do not have as much benefit as we had thought. Two recent articles on 3 omega fatty acids and vitamin D are examples. Researchers studied 3-omega fatty acid, 1 gram daily, used by volunteers over 65 years old for five years in a randomized double-blinded study looking for benefit in dry eyes. Dry eye disease was assessed at ophthalmology clinic visits. Between the group randomized to 3 omega fatty acids and those randomized to placebo, there was no difference in problems with dry eyes. The authors concluded that their research was “another disappointment for omega-3 fatty acid and dry eye disease.” The effort to prove 3- Omega benefit has been ongoing and repeatedly has failed.
In study of vitamin D supplementation, a randomized controlled trial with more than 20,000 people with normal Vitamin D levels published in the NEJM, showed that vitamin D supplementation did not have an effect on incidence of fractures, either vertebral fractures (spinal compression fracture) or hip fracture. We do, of course, recommend a Vitamin D supplement in persons with low vitamin D levels, because there is benefit.
For healthy people, especially those who go outdoors a few times a week or who have normal vitamin D levels, there is likely no need for vitamin D supplementation. Supplementation did lead to slightly increased bone mineral density, but this did not translate to reduced fracture risk.
Robert H. Kelly, MD FACP
QUOTES
Symptoms then, are in reality nothing but the cry from suffering organs.
Jean-Martin Charcot, M.D. 1868
Medicine has for its object the relief of suffering and the prolongation of life. There exist many limitations to the successful accomplishment of this object. The limitations of medicine are less numerous today than in the past, and many of the obstacles to success in the prevention of disease and the healing of the sick will be removed in the future.
The Editors, Journal of the American Medical Association, October 22, 1898
Every effort should be made not only to inculcate ethical ideals but to impress on a medical student the fact that success in medicine does not depend alone on exact diagnosis and successful treatment, and that in practice, you will have to treat patients, not cases.
The Editors, Journal of the American Medical Association, 1908
It is sometimes as dangerous to be run into by a microbe as by a trolley car.
James J Walsh, MD John Hopkins, 1910
I still find the most informative initial probe to be the simple query: “So, how are you feeling?
Robin Colgrove 2024
You are, once you sign up for (Medicare Advantage) plan, entering a complex contractual relationship with a for profit private company, and you must be able to discern what is best for you among the sleight of hand and obfuscation that is so rampant in medical care today.
Jerald Winakur, MD, 2024 Caring for the Ages, April 2024
A majority of physicians in the US are employees. Now, many also want to unionize. These doctors do not realize that they will miss out on one of the greatest lures of being a physician, that is, being your own boss.
Robert Doroghazi, MD, 2024
The quantitative fallacy: The human tendency to attach too much weight to factors that are easy to measure and not enough weight to more complex, hard to quantify variables. This inclination induces doctors and patients like to obsess over the crisp, objective, but highly nonspecific assessment of white blood cell count while ignoring the subjective impression of severity of illness as felt and seen by the patient, their family, and the physician.
Robin Colgrove, M.D., 2024
PMH STORY
The patient was over 95 years old and living in a nursing care center. A life-threatening infection developed. Breathing was difficult. She was treated at the facility and cared for skillfully by the staff. Dr. Kelly provided treatment for the infection, made appropriate medication changes, and monitoring. She recovered. Today was our first visit at her care center since her recovery.
It was early morning, but she awoke from sleep. With 2 reminders, she recognized it was Dr. Kelly visiting and she expressed her thanks for the visit. I spoke to her about her recent illness and recovery. She was thankful for her recovery, thankful for those who cared for her and thankful for her long life, children, and God’s grace. This was her character, to be aware of what is good in life and give thanks. We addressed her concerns and issues. I shook her hand to bid her goodbye. In response, she grasped mine with both of hers, saying, “I am so proud that you are my doctor.” This is the first time she had ever talked about being proud of anything. Her usual approach to life was one of humility and thanksgiving. She is a woman of clear thought and strong conviction though her health was Frail.
The role of a doctor in a frail, elderly person’s life is important, often a necessity, and hopefully a source of comfort. It was with humility that I received her good spirit, thankful for all life has granted her and all that she had done in her 90+ years. That was her spirit during the ten years I have been her physician. There are times when doctors may learn as much from patients as patients may learn from the doctor. And when we earn their endorsement, whatever word they choose, it is because we are serving them, and that is good.
Robert H. Kelly, MD FACP
A GOOD NIGHT’S SLEEP: DON’T DRINK ALCOHOL
Men with no sleep complaints and who were active and busy volunteered to sleep in a lab. They were asked to volunteer for two nights. Half of the men on the first night had no alcohol and on the second night received an alcoholic beverage before sleep. The other half of the men reversed: Taking alcohol in the first night. No alcohol in the second night. The researchers looked at sleep events with and without alcohol. Sleep events (apnea, hypopnea, and hypoxia), interfere with the quality of sleep. Sleep events chronically may cause illness.
The number of sleep events on nights with alcohol was twice as high as the nights without alcohol. Apnea events, where the individuals stopped breathing for a period of time, was five times more common after the alcohol than after the nonalcohol beverage. The severity of oxygen desaturation was significantly higher after the alcohol.
Even small amounts of alcohol periodically can have significant effects on health. That is why many organizations, like the American Cancer Society, now state: “It is best not to drink alcohol.” Certainly, if you want a good night’s sleep, do not drink alcohol before you go to bed. Sleep apnea and hypoxia are big issues in men’s health. It is surprising to me to learn that alcohol may play an important role in this common and serious medical problem. Most likely, women will have the same response. This research used men because sleep apnea is much more common in men.
Allan R. Kelly, MD FACP
EXERCISE: HOW MUCH TIME AND HOW MANY DAYS PER WEEK?
Researchers at Mass General Hospital in Boston published an observational study in JAMA this last month. They looked at activity characterized as vigorous, which would be similar to a brisk walk or leisurely jog, playing a sport like tennis, or working out in an exercise room. They looked at total amount of time and compared people who had more or less than 150 minutes of weekly exercise. They also compared outcomes in people who exercised only 2 days a week (weekend warriors) and those who exercised at least 5 days a week (regulars). 150 minutes a week is not so much. Just 21 minutes a day. It could be on an exercycle, a treadmill, or a walk around the block.
It turned out that the weekend warrior and the regulars got the same benefit. Specifically, people exercising more than 150 minutes a week compared to people exercising under 150 minutes per week, there was a 22% reduction in atrial fibrillation, a 27% reduction in the risk of a heart attack, a 40% reduction in the risk of a heart failure event, and a 20% reduction in the risk of a stroke. Similar results were seen with other exercise levels. For example, exercising more than 230 minutes per week gave the same results as exercising more than 150 minutes per Week.
Research confirms the value of exercise. For your well-being, you do not need to spend hours in the gym or running marathons. 20 or 30 minutes daily is more than enough. If you exercise two days a week, an hour a day is a good place to be. But this recent study once again indicates to get moving, it's good for you. Whether you are a regular or a weekend warrior, exercise reduces the risk of stroke and heart attack.
Allan R. Kelly, MD FACP
BRUSH YOUR TEETH
When you wake up in the morning, brush your teeth. We all are taught by our parents to brush our teeth. Certainly, the dentist gets after us. The bacteria in our mouth affects the overall ecology of the body and health. This may even have an effect on the risk of dementia. A study published in the December 18, 2023, issue of JAMA Internal Medicine looked at the association between daily toothbrushing and hospital-acquired pneumonia and death. The researchers looked at 15 randomized clinical trials of ICU patients. Most of the studies were done outside of the United States, and many were from China. We have known for some time that oral care has an effect on the sick and the elderly. The intervention was to brush the teeth two times a day in the experimental group, and no brushing of teeth in the routine care. After having worked in ICUs for decades, I have never seen a nurse brush a patient’s teeth. This is something new. The research showed that brushing the teeth two times a day shortened ICU length of stay by almost two days, and reduced mortality by 20%. Brushing the teeth more than twice a day in the ICU did not increase the value.
The accompanying editorial emphasizes the value of this report, Dr. Datta from Yale School of Medicine observes that there is, “compelling data that toothbrushing is an effective strategy.” So, here is something new for us to think about for our hospitalized patients: if they can’t brush their own teeth, perhaps we should brush for them.
Allan R. Kelly, MD FACP
HOW TO HELP PEOPLE WITH PAIN?
We are constantly trying to learn how best to help people with pain. Experimental trials continue to explore the role of different types of medication, therapies, and advice to help people get better control of pain. All of us want to help our brothers and sisters who are in pain.
There is increasing controversy about which medications are most helpful for pain. Back pain and neck pain are a common experience in life and can be disabling. Researchers in Europe published a report in Lancet, July 2023. They randomized over 300 patients with moderate-to-severe back and neck pain who presented to emergency rooms or clinics needing help with their pain. They were randomized to two groups. One group was given a placebo to take for their pain along with Tylenol or Advil or whatever else came to hand. The other group got the same advice for over-the-counter medications as well as oxycodone, a narcotic, at a medium dose of up to 20 mg daily. Pain was re-evaluated at six weeks. The average pain score was higher in the patients given oxycodone than in the patients given placebo. Adverse events were also higher in the group given oxycodone compared to the group given placebo. In other words, in patients who had pain severe enough to take them to the doctor’s office or the emergency room, giving oxycodone only made their pain worse and gave them more complications than giving them the same advice and a placebo.
Oxycodone in this human experiment was of no value in helping people with neck and back pain. Narcotics can help people have peace and comfort when they are suffering, distressed, or facing something bigger than they can handle. Morphine has been used for centuries. I believe that we know better today than we did just 10 years ago about how to use these drugs. The bottom line is that we are learning that we have used narcotics too much, too frequently, and with no discernible benefit to our patients who have neck and back pain. Research like this published in the Lancet will guide our care in the future.
The research is also a reminder how human experimentation can put our current practice in a different light. The doctors and the patients, the nurses, and the institutions that support human research help all of us to do better.
Allan R. Kelly, MD FACP
HEALTH EFFECTS OF CHILI PEPPERS
We remember the admonition – you are what you eat! When I was about 8 years old, that was confusing. It makes more sense today.
Peppers (e.g., relleno, chili) are common in many cultures. Are they good for you? The active ingredient of chili pepper, capsaicin, may carry some risk of adverse effects, including coronary spasm. What we humans do by cultural habit may at times be for our own good and at other times risky!
A recent observation study reported on chili pepper use and health outcomes. About one-quarter of the study participants reported taking chili pepper spiced foods at least four times per week, and they were compared to people reporting no or rare use of such pepper. There were confounding variables, including the observation that the chili pepper group more likely adhere to the principles of a Mediterranean diet and better diet quality (less processed meat). On the other hand, the chili pepper group tended to have higher blood sugars, blood pressure, and weight.
Mortality hazard was 23% lower in the high use chili pepper group compared to no or rare users. Reduction in stroke and cardiovascular mortality was 30-60%. There is no proof that this risk reduction was caused by chili pepper use. This is an observational study and does not at all prove chili peppers prolong life, but it is an interesting correlation. I wonder if it proves that healthier people prefer a spicier or more varied diet. Chili peppers fit into the basic laws of good nutrition: balance, variety, moderation, and they taste great.
Robert H. Kelly, MD FACP
MEDITERRANEAN DIET
The Mediterranean diet is a diet low in red meat, high in fresh fruits, vegetables, whole grains, nuts, olive oil, and tomatoes. 16 studies published from 2006 to 2021 were studied. Adherence to the Mediterranean diet was monitored. Stroke and heart disease were lower in the group that adhered to the dietary guidelines. This observational study may prove that people who are good at sticking to a program do better than people who cannot, especially if it is the diet patterns around the Mediterranean Sea and prudently restricting diet.
Another review of 30 controlled studies of sweeteners and sugar in the diet looked at cardiovascular mortality, diabetes, coronary events and death, heart failure, and stroke. In all of the studies published, there was a correlation between sweetener/sugar use with increased risk (10 - 20%). Health is affected by diet. Restrict sugars, enjoy fresh food in your diet!
Robert H. Kelly, MD FACP
QUOTES
“Novel procedures in medical practice find application so promptly in these days, that the scientific progress that they represent is all too often soon forgotten…[yet] The newest acquisitions to the healing art may sometimes become potential menaces until their limitations have been made clear.”
Editors, Journal of the American Medical Association, 1923
“I let that memory serve and inspire me to think of innovative approaches that will help make the distance and barriers between patients and clinicians smaller. I do not always succeed, but I try, I try to do something magical.”
Iyesatta Emeli, M.D., 2023
All too often, even the reputed scientist is found supporting a doctrine that is dangerously near uncertainty of demonstration, on the basis of inadequate investigation…the time has come when those interested in the dignity of science should protest, whenever it seems desirable, against any resemblance of finality or any assumption of authority in unwarranted statements of those who trade on scientific investigations.
JAMA Editors, July 21, 1923
“Every effort should be made not only to inculcate ethical ideals but to impress on a medical student the fact that success in medicine does not depend alone on exact diagnosis and successful treatment, and that in practice, you will have to treat patients, not cases.”
The Editors, Journal of the American Medical Association, 1908
“Misaligned quality measures can stifle clinical judgment and risk reducing the practice of medicine to mindless box checking. Over time, the number of quality measures has swelled to 2500, evolving into a confusing, time consuming and even soul crushing responsibility for the physician.”
Padmaja Patel, MD, 2023
PMH STORY
The patient’s spouse suffered cardiac arrest. Bystander CPR was not done. It was quite devastating to the spouse. 911 was called. CPR was initiated in the home.
EMS administered multiple doses of cardiac medications. Heart rhythm was restored in the emergency department. The patient was admitted by the cardiology and pulmonary team to the intensive care unit. Collaboration with and sometimes reliance on the teams at the hospital is becoming the usual course of hospital care. The PMH doctor will continue to visit, collaborate with the team, and assist. It is a professional, collegial, and collaborative effort. It is a change compared to 10 years ago.
Dr. Kelly went to the ICU to examine the patient and to meet with the family and ICU team. The ICU nurse and Dr. Kelly reviewed events and the patient’s exam and condition. The nurse was a 45–50-year-old experienced male ICU clinician. The nurse asked Dr. Kelly to talk to the wife, who was distraught. Before Dr. Kelly left, the ICU nurse stated, “I am so glad to see you, Dr. Kelly. You and your brother are God sends in cases like this, where there has been a severe and life changing event. The family knows you and you know the patients and can assess and communicate so well with the family.” I acknowledged this and went to see the patient’s wife.
Caring for ill patients, especially critically ill patients, is not a solo effort. Taking care of patients in the hospital is today best done as part of a team. This has become clear in the last year. However, the PMH physician will assist the patient, the family, and the team with continuing care.
Robert H. Kelly, MD FACP
DEMENTIA RISKS
A productive area of research examines how established, effective medications can have different and unlabeled long-term effects. Metformin is an excellent and inexpensive medication for the treatment of diabetes and can help fight obesity that is caused by other diabetic medications. Mayo recently published an important study done at the Veterans Health Administration and repeated at Kaiser Permanente comparing 2 common diabetic treatments – Metformin and Sulfonylurea – on the risk for developing dementia. They showed conclusively that metformin decreased risk of dementia compared to sulfonylurea. A more recent analysis confirmed this finding. The benefit may relate to reduced episodes of hypoglycemia. Metformin and sulfonylurea have been used for decades – now we know the choice affects the risk of dementia. Use the metformin!
Another recent report looked at cigarette use and dementia. Volunteers had cognitive testing in 1996-1998 and then had retesting in 2011-2013. The risk of dementia was 33% higher amongst smokers compared to those who had never smoked. Former smokers (who had quit in the interval between the two evaluations) had a 25% increased risk of dementia compared to those who never smoked. The conclusion was that as the time since quitting increased, the risk of dementia diminished. We have long known that smoking increases the risk of cancer and heart attack. Now we also know that smoking worsens dementia risk. Quitting reduces the risks. It is time to stop using these toxins.
Call if you need help.
Robert H. Kelly, MD FACP
HEARING LOSS and DEMENTIA
There has been talk in the last year or two about hearing loss having an effect on dementia, with the implication that it is a cause of impaired cognitive function or dementia. There is no science that establishes this link. Hearing loss and dementia are both signs of degenerative change. But cause and effect are less clear.
The Washington Post had in its headlines that “hearing loss is a major risk factor for dementia. Hearing aids can help” (10/2022). National Public Radio’s Weekend Edition said that there was a direct link between hearing loss and dementia and featured a scientist who said that hearing loss “actually affects the brain’s structural integrity as if people with poor hearing are also demented or will be soon. Some proponents of this viewpoint argue that hearing loss leads to a focal atrophy of the auditory cortex. There is no randomized trial to establish that cause and effect. The risk of stigmatization prompted the American Geriatric Society to combat the claim that hearing loss causes or worsens dementia.
Hearing better can help you communicate and interact more effectively in a social setting – maybe it helps you think better. Hearing aids can improve hearing ability, and so improve cognitive performance in those with dementia by reducing the extra work that impaired hearing imposes. But they do not change the structure of the brain. Whether it is Beethoven or Helen Keller, there need be no lack of intelligence in persons with poor hearing or who self-identify as deaf or use sign language for communication. There is no reason to say that people with impaired hearing have impaired cognition.
Robert H. Kelly, MD FACP
LESS IS MORE
Critically ill patients require nutritional support because they’re not eating. But often starting nutritional support leads to significant glucose abnormalities that require additional intervention like insulin to control glucose level. Then this can cause hypoglycemia, and hypoglycemia is dangerous and can cause death.
Research in the New England Journal of Medicine in September looked at the role of early IV nutritional therapy on outcomes.
The details are complex, but the conclusions are straightforward: early initiation of insulin was of no value to the patient, and the early initiation of IV nutritional support was counterproductive. As the editorial state: “Despite a century of insulin use in clinical practice, the ideal blood glucose target in critically ill patients remains unclear…” After over a century of use, there are still questions about how best to use insulin. The practice of medicine is constantly challenged by trying to do better. When we see that our current therapies are superior to more intensive, complex, and hazardous treatments, we are making progress. New is not always better. When it is, we will embrace it. When research shows us that the old is better, we are happy about that, too.
Allan R. Kelly, MD FACP
RISK FACTORS
The association of cigarette smoking with lung cancer was initially just an observation famously first published by Drs, Oshner and DeBakey in New Orleans. But further study showed causation in trials, both in animals and humans. Even though we have not had a randomized-controlled trial in human beings to prove that cigarette smoking causes lung cancer, the observational studies are so dramatic that we have confidence. Doctors continue to study what risk factors have the biggest effect on bad health outcomes. Researchers at Wayne State University’s School of Medicine in Detroit, Michigan report on observational studies done over 20 years in men and women first evaluated at 20 years of age. Looking at the extensive statistical analysis, three factors were highly associated with risk of stroke and/or death during 20 years of follow-up: Body mass index, blood pressure systolic over 130, and fructose consumption. In other words, what a person is doing at age 20 has an impact on the risk of trouble at age 40. The researchers went on to say that: “Risk increases exponentially with age.” Age creates risk, as do personal choices. Watch your weight and blood pressure. Cut the sugar way down.
Allan R. Kelly, MD FACP
PMH STORY
Continuity of care.
The patient is now in his 90s. When I first met this patient 20 years ago, he was oriented and alert, and he was pleased that I was his doctor. Why? Because my father had taken good care of his parents and that gave him a sense that he was working with someone he could trust.
Approximately eight years ago, his dementia began to take a toll. He started to call me by my father’s name, Gordon. Over the past few years, when he sees me, he greets me by name sometimes as Dr. Kelly, and sometimes as Gordon. He thanks me for taking such good care of his parents. He will call across the room, “Thank you Dr. Kelly for taking care of my parents.” As appropriate, I will try to reorient him, but his error is innocent and the reminder friendly.
What is it that makes people feel comfortable, cared for, grateful, good? Doctors, like nurses and other caregivers, want to provide that to our patients. It is complicated. In my life and career, I think continuing to give care over years is a part of the good that we can give to people, backed up of course by diligence, thoughtfulness, commitment, and quality. Continuity of care is important and reassuring. It helps doctor, patient, and family. People like knowing their doctor and his past work.
Allan R. Kelly, MD FACP
QUOTES
“In the 2022 National Geriatrics Fellowship Match, only 177 positions were filled out of 411 positions offered: 43%, the lowest percentage of all fellowships across 71 specialties of medicine. That is because geriatric medicine is one of the very few specialties for which fellowship training and board certification result in lower salary than if neither had been pursued…the median salary of geriatricians is 4% lower than that of general internist and 14% lower than that of hospitalist.”
Jerry Gurwitz, M.D., 2023
“Residency has shown me how pervasive the feeling of powerlessness is in medicine: physicians often do not have the answers patients desperately seek; but they are not powerless. They can always choose to treat patients with dignity and compassion.”
Julia Wagner, M.D., 2023
“Failing to implement telemedicine widely will result in patients losing the virtual option for medical care, leaving them unnecessarily burdened with in-person visits… Outpatients prefer telemedicine over brick-and-mortar clinic visits. Clinicians must be free to construct their outpatient telemedicine visits in such a way to meet the needs of the patient as well as the clinician.”
Stephen Klotz, 2023
PMH STORY
Ten years ago he was a new patient. In his early 80s, he looked stronger than usual. But as I listened to his lungs on the first visit, there was a problem. A chest x-ray showed a chronic disorder called bronchiectasis, with risk for serious pulmonary complications, respiratory failure, and reduced life expectancy.
The first few months, we used antibiotics to get the chronic infection under better control and started breathing treatments. He was great for this. But I saw multiple other areas where he was not following recommendations, and in our meetings, he was willing to accept some advice, but was relatively strict in rejecting other advice, like getting consultations. His daughter was a physician. I asked her about her father's strong mindedness, and she said she had no idea what to do about it, as he had always been that way.
As years passed, illness at times raised the question of hospitalization, consultation, and more complicated treatment. Repeatedly, he declined care at the hospital or in the emergency room and insisted on care at home. I spoke to the physician daughter, and she said she understood and that there was nothing she could do. I learned that this man’s decisions were working out for him. Though he had serious lung disease, he was at home, and made his own decisions.
This spring, he had another episode of pneumonia. The vital signs, laboratories and exam all indicated the need for hospitalization. I drove him to the emergency room, where x-rays and laboratories confirmed a serious pneumonia. But then he left the hospital against medical advice. I spoke to him before he left the emergency room. He made clear his preference, and I provided antibiotics to support him in his choice for care at home. He got better. Several months later, he is back to baseline and in good Spirits.
Doctors learn from their patients and choices. Occasionally, there are times when perhaps there is only one right way, but many medical decisions are best guided by the doctor and the patient working together honoring the patient’s goals and choices. In my prior practice experience, it would have been very hard to care for this self-directed, hospital avoidant gentleman. PMH gives the patient and doctor time to understand each other, make mutual decisions, and have plenty of time to respect the patient’s Choices.
PMH allows doctors, patients, and families to understand each other’s choices and wishes better. That is good for the patient, the doctor, and the family.
Allan R. Kelly, MD FACP
ADDING SALT AT THE TABLE
It is generally accepted that the Western diet is too high in sodium. A study in England using the computerized health records of 500,000 UK citizens looked at the impact of adding salt to food at the table. Using salt while cooking was not a factor, but just the response to one question “Do you add salt to your foods?” The answers could be no, usually, or always. Those who always added salt to their food showed the average life expectancy for women was 1.5 years lower and life expectancy for men was 2.3 years lower. Amongst the obese subjects, the relationship was less clear.
There may be other reasons for the results. For example, people who always add salt may be accustomed to a saltier diet or more snack foods. The conclusion remains: people who “always” added salt to their food had decreased survival and probably decreased quality of life.
Robert H. Kelly, MD FACP
DEMENTIA, HEALTH, & COMMON SENSE
Bruce Miller, M.D, a neurologist at University of California, San Francisco School of Medicine lectured on “dementia and primary care.” Dr. Miller introduced his colleague, Stanley Prusiner, M.D., a Nobel Prize laureate, and neurologist. They discussed modifiable risk factors for dementia. Dr. Miller discussed that alcohol consumption is a risk factor for Alzheimer’s disease and dementias, even one drink a week. Other top factors included head injury (falls), pollution, low education, hypertension, smoking, hearing impairment, obesity, depression, sleep, and physical activity. “Protective” exercise was defined as 45 minutes a week. Exercise correlates with brain connectivity and reduces inflammatory biomarkers and impaired function. Dr. Miller also discussed how “intuitively” he did not feel right if he did not get exercise.
Another recent report looked at tobacco use and dementia. The incidence of dementia was based on cognitive testing in 1996-1998 with retesting in 2011-2013. Risk of dementia was 33% higher amongst current tobacco users compared to those who never used tobacco. Those who quit in the interval between the two evaluations had a 25% increased risk of dementia compared to those who never used tobacco. The conclusion was that as the time since quitting tobacco use increased, the risk of dementia decreased. It is never too late to quit using tobacco.
If good health is the goal, whether using intuition, common sense, the recommendations of a royal commission, or the advice of a distinguished professor of Neurology at the University of California, there are things we can do that yield better health: use no tobacco or alcohol, avoid sugar, reduce falls/head injuries, get more exercise, sleep, and education. It is common sense and scientifically valid that we injure our brain with substances, pollution, injury, and ignorance.
Robert H. Kelly, MD FACP
DIABETIC PERIPHERAL NEUROPATHY
A study of 68 persons with diabetic peripheral neuropathy (DPN) was published in 2021. Standard treatment for peripheral neuropathy included gabapentin, Lyrica or amitriptyline. In a randomized blinded fashion, one-half of the group were treated with vitamin D 5000 units daily and the other half were treated with a placebo pill. Neither group knew what the pill was, nor was supposed to be, other than it was a treatment for neuropathy pain. Satisfaction with treatment was then measured eight weeks later. The differences were significant and noticeable to patients. With regard to measuring the mood of patients, there was an improvement in mood in 88% of the patients given vitamin D, and 70% of the placebo patients. Pain was improved by 1 point on a 100- point analog scale, not clinically meaningful. There are many reasons to consider a vitamin D supplement. Helping people feel better is a good one.
Robert H. Kelly, MD FACP
SUGARY DRINKS…AND DEATH
There has been concern that sugar use is not good for us. There have been very few randomized control trials, to prove causation, but many observational studies showing Association.
An important example of this observational research was published in the British Medical Journal in April 2023 based on the nurses’ health study which began in 1976. The study enrolled 122,000 female registered nurses aged 30 to 55. It was supplemented in 1986, including 52,000 male health professionals, largely physicians. In the study, participants with a new diagnosis of diabetes were selected. Researchers looked at how the use of sugar beverages changed after the diagnosis of diabetes. Many different beverage types were studied: Sugar-sweetened beverages, artificially sweetened beverages, fruit juice, coffee, tea, low-fat milk, full-fat milk, plain water, caffeinated, caffeine free, carbonated, and noncarbonated. To avoid confounding, scores of other variables were also studied.
The results were specific and notable. The use of sugar-sweetened beverages after the diagnosis of diabetes increased mortality significantly. The increase in the use of coffee, tea, and plain water as well as low-fat milk products benefited mortality. Increasing the use of coffee, tea, and plain water after the diagnosis decreased the risk of death. The magnitude of risk was a 20% increase in the risk of death by increasing sugar-sweetened beverages by one beverage per day on average. Increasing the use of coffee, tea, or plain water reduced the risk of death by a factor of 20 to 30%. The table shows all-cause mortality data from this experiment. It is a reminder to reduce the use of sugar-sweetened beverages (SSB) and artificially sweetened beverages (ASB). It is a reminder that coffee, tea, and plain water are probably good for you, compared to other beverages. And it is also a demonstration of endurance and good research: The nurses’ health study has been with us for 45 years, and we continue to learn from it. Bravo to whoever initiated the nurses’ health study so many years ago.
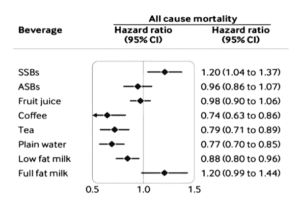
Allan R. Kelly, MD FACP
SURGE IN CASES OF SYPHILIS
JAMA reports that syphilis cases surged in the United States from 2019 to 2021, increasing 32%. Also, the editors note the increasing numbers of hepatitis B and hepatitis C infections in an era when treatment is available, and vaccines are widely administered to younger people.
Vaccines and treatments save lives. But we also know that certain behaviors increase the risk of infection and death: Age of onset of sexual activity, promiscuity, drug use, especially intravenously, alcoholism, and cigarette use are examples.
Authors from Harvard and the Coalition for Global Hepatitis elimination, opined as follows: “The plan developed by representatives from across the Department of Health and Human Services with input from multiple external partners, recommend 55 major strategies and some 150 specific government wide actions to prevent new infections and improve early diagnosis and treatment of viral hepatitis.”
The authors state that the incidence of hepatitis infections has doubled since 2013 despite the availability of curative medical treatment.
Nowhere in the articles is there any mention of the risk factors that so markedly increase disease transmission: Promiscuity, sex with high-risk partners, and the use of drugs and alcohol.
As a physician, I want my patients to know that there are many simple things they can do to promote their health and well-being. Whether or not, the 150 specific government actions or the 55 major government strategies can improve the health of these brothers and sisters, I am unsure.
Allan R. Kelly, MD FACP
QUOTES
“To the insulin committee of Toronto, and through its recommendation to the Eli Lilly Company, I have been indebted for the rare privilege of using insulin. For this, I cannot be grateful enough.”
Elliot P. Joslin, M.D., 1923.
“If we are not careful, we might even convince society that the electronic medical record, and what it represents, is an end in itself, it is more important than taking care of the sick, training our successors, and finding cures for human disease. Or is it already too late? Do you read me, HAL?” Instead of supporting clinicians seeking to deliver care more effectively and efficiently, current EHR [Electronic Health Record] design and configurations, attempt to manage clinicians and how they do their work. The deterioration in the patient-clinician relationship and increased clinical burden are often blamed on the EHR.
Don Dentmer, M.D. 2023 JAMA
PMH STORY
A patient with substance use problems developed serious complications. He was ill in a hospital out of state, cared for by medical school faculty. It was a difficult four-week hospitalization. Heart disease was identified, treatment was given, and he returned to Texas.
Dr. Kelly reviewed the medical center records. There was a need for local cardiology follow-up, which was arranged to be done the day after the patient’s next visit with Dr. Kelly.
The patient visited Dr. Kelly. And he explained that further consultation was possible. Dr. Kelly said that the specialists involved with his care were members of a large university group. The cardiologist group in town was also a big group. With the referral, Dr. Kelly assured the patient that both the university group and the Fort Worth group were excellent and sophisticated. Dr. Kelly said, “As you know, I am not a member of a group.” Without hesitation, the patient said, “Dr. Kelly, you don't need a group.” PMH does not substitute for a University Medical Center. PMH does not substitute for a group of skilled cardiologists. What PMH does is provide ready and convenient access to an expert physician who knows the patient’s case, who understands the patient’s care, and who collaborates with other physicians to meet the patient’s needs. And sometimes what the patient needs is the one physician. Having a Premium Medical Home can help achieve important goals.
Robert H. Kelly, MD FACP
AT HOME TESTING
We have learned from the COVID epidemic that at home testing helps people and doctors. We know how important at home testing for pregnancy has been, helping women make better decisions and understand what is happening with their bodies. At- home testing for COVID has also helped people to understand why they have a fever or why they do not feel good. You do not always need a doctor to understand why you do not feel good or to understand what is happening with your health or your life.
The FDA has now authorized, for the first time, an over-the-counter home diagnostic test to detect Influenza A, Influenza B, and COVID. Based on our experience for the past three years, this is a good move. It is good to make testing available to individuals who have knowledge, capacity, and motivation to do their own testing. Once they get their test result, then they can make a decision how they want to proceed. Many adults will not want to do their own testing, but they have that choice. When it comes to potentially treatable diseases like influenza, home testing will help people make good decisions.
Allan R. Kelly, MD FACP
HUMAN STOOL AS A SOURCE OF MEDICAL TREATMENT
The development of antibiotics has helped people in many ways and prevented many deaths. But the use of antibiotics occasionally causes distortions in the normal human microbacterial ecosystem. At times, these adverse effects of antibiotics in the colon ecosystem lead to opportunistic and potentially deadly infection of the gut, an infection called Clostridium difficile colitis. C. difficile infection can also lead to colon removal to save the patient’s life.
This clostridium infection, a complication of antibiotic therapy, has traditionally been treated with other antibiotics. In other words, a problem created by antibiotics is treated with antibiotics. Unfortunately, relapse is common.
Approximately 10 years ago, a series of experiments showed that this type of infection can also be treated simply with stool. The details are complex, but essentially a healthy family member can donate their own stool to a person sick with clostridium disease. These stool infusions, or “transplants,” are accomplished with colonoscopy. Stool treatment saves lives and prevents relapses.
Further analysis of what was in the stool that saved the lives of the sick has led to development of bacterial capsules to prevent relapses and cure the infection. Capsules containing multiple strains of benign Clostridium species are taken once a day for 14 days orally. Compared to placebo capsules, the use of these Clostridium capsules reduces the risk of infection by 75%. The study was published in JAMA 2023 by researchers from Canada and United States.
Living microorganisms can be used to help fight infections caused by other microorganisms. This breakthrough represents an important new frontier.
Allan R. Kelly, MD FACP
LYMPHOMA, CHEMOTHERAPY, AND HEART FAILURE: STATINS HELP
We have known for decades that the use of statin drugs, like rosuvastatin or atorvastatin, saves lives in people with coronary artery disease or who are at increased risk for a myocardial infarction. But how about people who do not have coronary artery disease, and who are at average risk of cardiac events? The research presented at the American Heart Association meeting included a randomized controlled trial of 300 patients with lymphoma. Lymphoma chemotherapy causes heart failure in a significant percentage of patients. But lymphoma is a fatal illness. Cure of lymphoma can open up decades of life that would otherwise be lost. How can we reduce the risk of heart failure in our lymphoma patients treated with certain chemotherapies?
Researchers asked: If statins prevent heart disease and heart deaths in high-risk populations, how about patients exposed to high-risk chemotherapy? The problem with chemotherapy is heart failure, not heart attack. In the experiment using volunteers with lymphoma on certain chemotherapies, one group was randomized to receive a statin, in the other group a placebo. The researchers studied cardiac ejection fraction as a measure of the strength of the heart. In the group treated with placebo, 22% had a significant reduction in the strength of their heart. In the group treated with statin, only 9% experienced a reduction in strength of heart function.
This research extends our confidence that statins can help protect the heart. We have gone beyond coronary artery disease (heart attacks), and now add chemotherapy side effects: threats to the strength of the myocardium. Statins have been on the market for 40 years. They are inexpensive, and widely available. They protect the heart. It is remarkable how we learn new things about old products that can save lives.
Allan R. Kelly, MD FACP
DECREASING ROLE FOR OPIATES
A study in Australia asked if morphine could reduce breathlessness in persons with moderately severe COPD. In the 20 th century, morphine (and opiates) became a go to solution for persons suffering symptoms of chronic disease. A person acutely short of breath, as with heart attack or heart failure, is quickly comforted by IV morphine. The theory was that morphine would relieve breathlessness and improve quality of life in patients with chronic breathlessness caused by COPD/emphysema. This was not widely used because of restrictions on opiate use, but it was a theory. The Australian study tested this.
The study compared people in the community who became short of breath while dressing or after walking 100 yards on a level field. They were not using continuous Oxygen.
Doses of 8 mg - 32 mg of morphine (extended-release preparation, or ER) were compared to placebo. The morphine dose was started at 8 mg and 16 mg and increased in two steps to a total dose of 8 mg, 16 mg, and 32 mg ER morphine daily.
Comparing those treated with morphine to those on placebo, there was no difference in how many steps were taken in an average day or in complaints of breathlessness. However, there was a difference found in hospitalization and death. In the morphine group approximately 33% of persons died or required hospitalization, whereas in the placebo group 18% died or were hospitalized.
Morphine has a role to play in acute suffering, at the end of life, and to treat postoperative pain. But the role of morphine and opiates in long-term pain control, breathlessness, and other symptoms of chronic disease is problematic. Except at the end of life or after trauma, opiates are generally not beneficial.
Robert H Kelly, MD FACP
THE MEDITERRANEAN DIET AND SUGAR
The Mediterranean diet is a diet low in red meat but high in fresh fruits, vegetables, whole grains, nuts, olive oil, and tomatoes. Sixteen studies published from 2006 to 2021 were reviewed, mainly conducted in the United States and Europe. Adherence to the Mediterranean diet was monitored by reported diet. Stroke and heart disease were lower in the group that adhered to the dietary guidelines. This observational study may prove that people who are good at sticking to a program do better than people who cannot, especially if the program resembles the diet patterns around the Mediterranean Sea and prudently restricting diet.
Another review of thirty controlled studies of sweeteners and sugar in the diet looked at cardiovascular mortality, diabetes, coronary events, death, heart failure, and stroke. In all of the studies published, there was a correlation with an increased risk of 10% to 20%. Our grandmothers might have said, you are what you eat. Health is affected by diet. Restrict sugars and enjoy fresh food in your diet!
Robert H. Kelly, MD FACP
STATINS AND BRAIN DISEASE
Researchers studied 3,000 adults free of dementia and Parkinson’s Disease (PD). During six years of follow-up, 50% of the adults in this British study (of elderly at risk of brain disease) went on to develop PD. After controlling for risk factors and other diseases, statin treatment was shown to reduce the risk of Parkinson Disease by 16%, even more so with the high intensity statins like Atorvastatin and Rosuvastatin. Postmortem examination of brain tissue looked at cerebral atherosclerosis. Statin treated brains had a 37% reduction in burden for atherosclerotic changes. The researchers concluded that statins reduced the risk of Parkinson’s Disease and vascular disease in otherwise healthy older adults.
Robert H. Kelly, MD FACP
QUOTES
The physician who makes all possible use of his daily clinical opportunities learns something new and useful every remaining day of his professional life. The daily clinical observations fortified by selective reading and standard textbooks and good medical journals afford a method of self education of the greatest value.
Frank Billings, M.D., 1923
“I sometimes wish every physician could understand the loss of a child. I wish they could understand how I miss (my daughter) achingly how I miss her in my bones… I wish every physician could understand - without going through the unimaginable - that our success in this profession is not defined by achieving external validation metrics, but rather by our ability to care for and about our patients.”
Ethan L. Sanford, MD, 2023
“I did perhaps the most important thing possible as a physician; I listened.”
Ferdinand Venditti, MD, 2023
Regardless of what the future holds our analysis demonstrated that increased consumption of sugar, sweetened, and possibly artificially sweetened beverages is a detrimental factor on cardiovascular health.
Chaya Krittanawong, MD, 2022
PMH STORY
A patient’s lab tests showed blood in the urine. Because of risk factors (including cigarette smoking and some toxic exposures) there was concern for cancer. Initial testing of the urine showed possible cancer. Referral was made to urology and the patient was scheduled for a consultation approximately 30 days later.
Two weeks before the consultation, the patient found himself on the road to go to an appointment in the morning and he was not quite sure where the appointment was. He called his PMH office. Review of his chart showed no known appointment set for that day. We called two offices where he visited, but neither showed an appointment scheduled for him that day. We called the urology office, but early in the morning they did not answer the phone and the answering service could not answer our question. Dr. Kelly recommended that the patient go to the urology office in case that is where the appointment was set.
An hour later, Dr. Kelly got a call from the urology office secretary. The receptionist said, “His appointment is for the end of the month, about two weeks away.” Dr. Kelly explained the situation, accepted the planned appointment, and thanked the receptionist for helping him. Dr. Kelly figured the patient would be asked to return for the previously scheduled visit.
Several hours later, Dr. Kelly received a copy of a consultation note done that same day from the urologist. With the patient there in the office, although his appointment was scheduled some weeks later, the urologist evidently saw the opportunity, discomfort, and need and basically said, “Let us get to work.” The urologist’s office did a good job. This is not so much a PMH story as it is a story of good care. It is good to be reminded of how things ought to be, and how things sometimes are. Our community can be one of the world’s best medical communities.
That was a good day for PMH.
Robert H. Kelly, MD FACP
FLU VACCINE REDUCES RISK OF DEATH
Flu vaccine saves lives.
We are accustomed to getting our flu vaccine. We are told it makes a difference, helps us to avoid hospitalization, and reduces the risk of wintertime death. Researchers in Sweden randomized 2571 volunteers who had survived recent heart attacks and were hospitalized. They were recruited through the study from 2016 to February 2020. The average age was 60, and 82% were male. None of the participants had had a flu vaccine for that year prior to the myocardial infarction. Half of the volunteers received a flu vaccine before hospital discharge. The other half got a placebo. During three years of follow-up, all cause death rate was 41% lower in the influenza vaccine group compared to the saline placebo group. The author of the study, Dr. Frobert, was quoted: “Patients with cardiovascular disease should get their annual flu shot…a flu shot could prevent cardiovascular death…”
There is general acknowledgement that flu shots are prudent. It is remarkable to see a placebo-controlled flu vaccine experiment study. The 41% reduction in death rates in persons with recent heart attack is surprising. Whether this result could be recreated in the United States, we don’t know. The experiment shows that an annual flu vaccine for our patients with vascular disease will likely save lives.
Allan R. Kelly, MD, FACP
LUNG CANCER SCREENING
The benefit of lung cancer screening is not as great as we would want. It leads to about a 20% reduction in lung cancer mortality. The United States Preventive Services Task Force has revised its recommendations for lung cancer screening. Prior recommendation applied to people 55 - 80 years with more than 30 “pack year” history of tobacco use. The new recommendation is people 50 - 80 years with a 20-pack year history. A third element includes persons who had been smoking within the last 15 years. Persons 50 – 80 years old who have been smoking in the last 15 years or who have smoked on average more than one-half pack a day for 30 or 40 years (or one-pack a day for 20 years) should have an annual CT scan of the lungs.
Finding a nodule or suspicious area on a CT screening exam does not mean that there is lung cancer. A normal scan does not mean there will not be lung cancer. As many as 20% of scans will have an abnormality that is not cancer. Newer evaluation processes have reduced the problem of false positives. About 1:20 patients who have a nodule found at CT lung cancer screening will have lung cancer at an early stage. So, if there is an abnormality, remember there is about a 5% chance that the abnormality will be lung cancer. If a smoker has a normal scan, there is a 98% or better chance that they are free of lung cancer at that time. CT screen is not perfect, but it is a path to decreased death rate from lung cancer.
Robert H. Kelly, MD FACP
MORE ON PAIN RELIEF
Researchers at the Hennepin County Medical Center, Minneapolis did a double-randomized crossover trial. They subjected volunteers to pain from an ice-cold bath. The hand was placed in the ice bath for a period of 10 minutes and the severity of pain was indicated on a visual analog scale that was 100 mm across. The participants were asked to rank their pain at different times on that scale with their hand in the ice-cold Bath.
In the experiment, volunteers were exposed to multiple drugs: Tylenol alone, Tylenol plus hydrocodone (Vicodin), ibuprofen, and placebo.
With placebo, there was no change in pain compared to the pain experienced before administration of the blinded drugs. The pain relief with Tylenol was statistically significant and consistent, 10 mm on the visual analog scale. A reduction in pain from an average of 50 to an average of 40. Reduction with hydrocodone plus acetaminophen was the same, a reduction from 50 to 40. Interestingly, with the ibuprofen, there was no change in pain. and there was no placebo effect. In other words, pain experienced with ibuprofen and placebo tablets was the same as pain experienced without any premedication whatsoever.
All of us are familiar with popular pain pills that were marketed as acetaminophen with hydrocodone or acetaminophen with oxycodone, like Vicodin or Percocet. These drugs were marketed for years. But this research from Minnesota on healthy volunteers raises the question: Was the pain relief from these popular narcotic drugs achieved by the acetaminophen, with no significant added benefit from the narcotic? This research says it is so. Interestingly, the volunteers were asked about side effects. No side effects were experienced with Tylenol, ibuprofen, or placebo. But approximately half of the patients given the hydrocodone did experience side effects including nausea and Fatigue.
This was a small study but is indicative of research over the past several years that calls into question the value of narcotics for people with postoperative pain or acute pain.
Allan R. Kelly, MD FACP
REDUCE DEPRESSION AND ANXIETY: REDUCE SOCIAL MEDIA
Researchers in England report a randomized control trial looking at counseling patients on the use of social media. Volunteers recruited in Bath, England, were interviewed regarding their use of social media. The volunteers were then randomized, one group was counselled to stop using social media, specifically Facebook, Twitter, Instagram, and TikTok for one week and then to continue to use social media as usual. At the one- week follow-up, the group counseled to stop using social media for one week had a significant improvement in well-being, depression, and anxiety. The magnitude of benefit was correlated to the reduction of self-reported minutes on Twitter and TikTok, especially TikTok. The author’s comment: “The present study shows that asking people to stop using social media for one week leads to significant improvements in well-being, depression, and anxiety. Future research should extend this to clinical populations and examine effects over the long-term.”
Should I say, “stop using social media?” There is much left to learn, but it’s not a bad thought.
Allan R. Kelly, MD FACP
SYMPTOMS ARE COMMON
A study of Medicare beneficiaries over age 65 looked at how often symptoms occur. They found that in community-living population, only 1 of 4 had none of the common symptoms that were monitored: pain, fatigue, breathing difficulty, sleeping difficulty, depressed mood, and anxiety. Of the 75% of the community-dwelling older adults who had symptoms, nearly half had two or more symptoms and 14% had four or more symptoms. Symptoms are common and not always a sign of disease.
Pain and fatigue were the most common co-occurring symptoms reported by 32% of individuals. The most common triad of symptoms was pain, fatigue, and sleep difficulty in 13%. Decreasing independence in daily activities and mortality correlated with Symptoms.
We live with these common symptoms in our daily lives. It is when new symptoms arise and persist, or when old problems worsen, that we are more likely to ask a doctor for advice. But these common symptoms may not respond to treatment. Healthy people commonly experience irritating symptoms with no pathological cause.
Robert H. Kelly, MD FACP
QUOTES
100 years ago, the total per capital consumption of sugar in the United States was less than 9 pounds a year. It has increased by leaps and bounds, until now, this country is probably the largest consumer of sugar in the world...
[Written in 1922. Since then, sugar consumption has continued to increase to more than 100 pounds per year.]
The editors, JAMA, 1922
The doctor as a private physician working for himself is more and more disappearing, but there will be general practitioners in out-of-the-way places as there are now; there will be men of rare talent and ability who will attract by their personality and who will remain individualistic in their work…
The editors, JAMA, 1897” [yes, 1897]
If a doctor has himself been the victim of a certain malady, forever afterward, is he more particularly interested in that affliction, and more sympathetic toward anyone so afflicted.
JMT Finney, MD, 1923
Our patients decide how to integrate our recommendations into their values and worldview, it then becomes our job to care for them with both empathy and humility, recognizing that we cannot really know what we would do if we were in their shoes.
Richard E. Laiter, MD, 2022
Physician independence has always meant more than an economic status. It has been the foundation of a professional ethos that imbues a dedication to science, a devotion to patient welfare, and a broad commitment to the health of the public. Critically, the medical and moral authority that physicians had rested largely on professional sovereignty.
Kevin A. Schulman, MD, 2022
It usually requires a considerable time to determine with certainty the virtue of a new method of treatment and usually still longer to ascertain the harmful effects.
Alfred Blalock, MD, 1899-1964
PMH STORY
The PMH member had a fall at home. He lives out of town. There were chronic medical issues that were stable on treatment. Dr. Kelly recommended X-Rays and an exam at a nearby urgent care center. Dr. Kelly asked the member to give me a call on arrival at the clinic. Upon arrival, he called and handed the phone to the clinic doctor. The doctor and I were acquainted and were able to exchange information about medical issues and plan for treatment for the injury. The patient was released.
Similirly, a patient’s family member called today. They were alarmed because the patient had been taken from a rehab center to a hospital south of Fort Worth. Family members were worried about the condition of their loved one.
This hospital is on Epic electronic record platform where Dr. Kelly has privileges, so Dr. Kelly was able to call up the data and bring the patient’s family up to date on the current events and status. This immediate information to the family helped them be aware and involved in events. This was reassuring and effective for continuing care.
It is both the availability of the doctor and access to information that is a benefit to PMH members and their families. Information may be available in other settings, but the doctor may not have time. Or the doctor may not know the patient and family. A call to many offices must work through layers of intermediaries - computer messages, nurses and on-call staff may have little insight to share. PMH’s direct and timely access to information and collaboration for planning is what patients and families want. PMH’s commitment to availability, being not too busy, makes a difference. This is what PMH offered to these two patients on one day in October. It is what we seek to offer every day that it is needed.
Robert H. Kelly, MD FACP
CAROTID ARTERY STENOSIS
Between 1995 and 2010, several studies were published concluding that the optimal treatment of asymptomatic carotid disease was surgical repair or endarterectomy. Endarterectomy carries an immediate risk of postoperative stroke in the order of 1% or more. These prior studies followed patients for 5 years and were randomized. The incidence of stroke was reduced in patients undergoing surgery.
A 2021 retrospective JAMA study looked at about 4,000 patients in Kaiser Permanente Northern California with severe carotid artery stenosis on one side, discovered on x-ray between 2008-2012. The patients were then followed through 2019 for incidence of stroke. The average age was 74, so the Kaiser patients were older. All-cause mortality from 1995 to 2019 was 55%, consistent with older age. Controlling for other issues, the 8-year risk of stroke was 2.7% even though no surgery was done.
The risks now are much lower than what was reported in surgical studies in the 1980’s and illustrate how medical treatment has changed the natural history of carotid stenosis. Treatment for asymptomatic carotid stenosis with statin drugs, blood pressure control, nonuse of tobacco, and metabolic control apparently reduces stroke risk to less than 3% over eight years of follow-up.
Robert H. Kelly, MD FACP
HALF EMPTY OR HALF FULL?
In 2021, The American Heart Association recommended addressing psychological health in its assessment and management of patients at risk for heart disease. Articles from 1995-2005 addressed the association between heart disease/mortality and optimism.
The data showed a 10 to 20% reduction in mortality and cardiovascular risk in persons objectively assessed as having an optimistic view of life, also called positive psychological health. Previous case reports and studies have documented adverse effects of anger/pessimism and health outcomes.
Benefits of optimism may relate to stress hormone response (e.g., cortisol and adrenalin). Some of the studies actually looked at the specific anatomic areas of brain function and blood levels of stress hormones -- they found favorable correlation with positive attitude or Mood.
There is no pill that can instill optimism or psychological health. Or is that what a placebo does after all! But we might look at our responses in life and consider that a positive response may do our own health better than a negative response. And there is the impact on others. The reports on optimism are a reminder that mindset and choices can impact our health.
So, the analysis suggests that those with optimism have reduced mortality. Maybe it was just intuition - those with negative outlooks were aware that their health was not as good. Or maybe optimism has an effect on our underlying health. The data suggest that choosing a path of optimism and turning away from anger is good for your health.
Robert H. Kelly, MD FACP
HIGH-DOSE FLU VACCINE SAVES LIVES COMPARED TO LOWER-DOSE
The researchers studied a Danish vaccination program. In some parts of Denmark, both high-dose flu and regular dose flu vaccines were available, and in other parts of the country, only the regular flu vaccine was available. It was not a randomized trial with a placebo control but comparing groups in different parts of the country where different vaccines were available. Regions with the high-dose influenza compared to regions with only the standard influenza vaccine, showed a 49% reduction in the risk of death in the
subsequent flu season, and a 64% reduction in the risk of hospitalization for influenza or pneumonia. There was no significant difference in adverse events in the two groups. The Danish medical research establishment is leading the way with new insight into the use of influenza vaccine. We recommend influenza vaccine for our patients during flu season. There can be complications from flu vaccines. But looking at endpoints like death and hospitalization, flu vaccination is likely beneficial for elderly people. Get your flu shots in the fall.
Allan R. Kelly, M.D.
HOW TO PROTECT THE KIDNEYS? GO FOR A WALK
Preventative care is important. 1199 seniors were randomized into two groups. One group went to weekly workshops for 26 weeks looking at a variety of health topics relevant to older adults but not physical activity (exercise). The intervention group participants were expected to attend exercise sessions at a center twice weekly and encouraged to pursue home-based activities three or four times weekly throughout the trial. The exercise goal was to achieve 150 minutes of walking per week. Strength, flexibility, and balance training were done 10 minutes twice a week. Participants were asked to walk somewhat hard.
There was no difference in weight or blood pressure in the two groups. The exercise intervention group was significantly less likely to develop significant decline in kidney function. As a physician, I would not typically expect to see a change in kidney function based on randomization to an exercise group versus a non-exercise group. This observation adds to the benefits of encouraging exercise.
Prior research showed reduction in the risk of heart attack, stroke, and death compared to peers who are not instructed and encouraged to participate in exercise. Members can call the PMH office, and we will help set them up with exercise training at a medical type of facility, like Carter Rehab Center at Baylor All Saints. Or, if you are strong enough, a simple 20-minute walk every day will make you stronger.
Doctors wear many hats. I don’t know what we will think if doctors start carrying whistles around their neck!
Allan R. Kelly, MD, FACP
PMH STORY
At PMH, we put great value on continuity of care. We believe that it is meaningful to patients, their families, to doctors, and nurses to have continuity of care. How this affects different people was seen in a recent emergency room visit.
The PMH doctor was already in the emergency room seeing another patient. He received a call from a son of a woman I called Sarah for this story. The son reported that his mother had lost consciousness and the caregiver had called 911. The PMH doctor finished his work and headed for EMS triage, where the ambulances come into the ER. As he was walking to the end of the hall, he saw Sarah. Paramedics on either side were bringing the gurney down the hall. Well into her 90s, Sarah still recognized her doctor. She smiled. “Oh Dr. Kelly, it's so good to see you.” Dr. Kelly greeted her, and walked along with the paramedics, asking what happened and listening to her story. The nurse helped move the patient into the ER bed. While standing there, the paramedics turned to the doctor and gave a report of what they had found and measurements they had made. During this presentation, the ER doctor with scribe and a nurse walked up and listened. Dr. Kelly examined the patient and stepped out into the hall to talk to the emergency room doctor.
The ambulance crew followed and the older EMT said, “I’ve never seen this before in my life. I’ve never before seen a doctor who knew the patient and greeted the patient in the emergency room.” The EMT was impressed.
How about Dr. Kelly’s point of view? I can tell you; it is good to see a patient that I already know. I feel responsibility and compassion for my vulnerable and ill patient. So, whether it is the patient, the EMT, or the doctor, all see value in this continuity of care. Why is it uncommon? The emergency room used to be full of doctors seeing their own patients, patients they knew from their offices and prior hospitalizations. But, for the most part, those days are gone. In our work at PMH, we continue to value continuity of care in the office, the emergency room, hospital, or on the phone. We believe continuity of care is good for patients, families, and our colleagues.
Allan R. Kelly, MD FACP
QUOTES
It is a most gratifying sign of the rapid progress of our time that our best textbooks become antiquated so quickly.
Theodor Billroth, MD, 1872
It is believed that the medical professional finds this bedside telephone a great convenience to themselves and to their patients.
Ae Rockey, MD, 1922
Despite early successes in improving patient’s safety and hospital performance, outpatient metrics obligations have exploded without evidence of benefit. For though such efforts might identify people for whom we can meaningfully intervene, examining seemingly beneficial requirements in isolation risks overlooking the cumulative toll that check the box approach to medicine has taken on clinicians and patients.
Lisa Rosenbaum, MD, 2022
The hospital - when you spend so much time there - tends to breed an insular, almost provincial mindset. As we chase troponins and analyze pixelated MRIs, we too easily lose sight of the real stories, the ones that matter most to our patients, their families, their communities, and their shared human history.
Sneha Mantri, MD, 2022
PMH STORY
In making rounds at the hospital, a great day is when the patient gets to go home. It is also a time when I reflect on what PMH is trying to do.
At discharge, we need to “reconcile” the medication list from the hospital with the patient’s pre admission medication list to identify needed home (discharge) medications. This process depends on the accuracy of the computerized pre admission list. It depends on the physician’s knowledge of the patient’s medical problems. It depends on communicating with the family about things like where to send the prescription, and who to call if there is a problem.
When the outpatient physician is also seeing the patient in the hospital, I believe errors and confusion are minimized. The doctor already has the pre admission medication list. The doctor is able to talk to the family and the patient about the discharge process, the discharge medications, and the discharge follow-up. The physician already knows which pharmacy the patient uses and can confirm it during rounds.
Most importantly, of course, the family knows who to call. The same doctor who saw the patient in the hospital would be responsible for the medications at home the next day and will be responsible for that medication list on follow-up in the doctor’s office. For patients and family members, medication lists are complicated. I remember trying to take care of my own parents. It was not easy to understand what medications they are supposed to be on in transition from hospital to home. These transitions are complex for family caregivers, patients, and doctors. Having a doctor involved with both the inpatient and the outpatient care will make this transition better.
Allan R. Kelly, MD, FACP
FALLS AND AGE
65 is the age when Medicare starts, and the Center for Medicare Service is interested in the health experience of its enrollees. The Current Beneficiary Survey has been done since 2010, recording health outcomes. In the 2017 survey, 45% reported a fall. Most of these falls did not result in significant injury.
Falls cause problems for people of any age. We should all be aware of steps that may reduce risk of falls:
- Exercise daily for at least 10 minutes.
- Reduce or eliminate alcohol.
- Report falls to your doctor.
- Balance classes at a local gym or YMCA, like Tai chi.
- If you have a serious fall, work with a physical therapist. Your doctor can write a prescription and Medicare will cover the cost.
- Make sure your home is safe. Look for places to put handrails, grab bars or other devices. Make sure the surfaces are flat and there is nothing on which to trip. Repair trip hazards before you fall or fall again.
Allan R. Kelly, MD, FACP
HEALTH AND SLEEP APNEA
Researchers in Spain studied 89 men with severe obstructive sleep apnea (OSA). The men were randomized to two groups.
The intervention group vigorously addressed nutritional change, moderate aerobic exercise for 20 minutes 5 days per week, smoking cessation, alcohol avoidance and sleep hygiene with weekly discussions lasting 60 minutes. The control group had a one time 30 minutes session to discuss these changes in lifestyle. Average age was 54. Average weight was obese -- BMI 34.
After six months, there was substantial improvement in the treatment group versus no change in the control group. After six months, in the treatment group, 29% of patients experienced complete remission of OSA and 60% no longer required CPAP. On the contrary, in the group without intervention, there was no improvement in the OSA scores or severity.
This adds to the understanding that consistent nutritional change, daily exercise, and non-use of alcohol can often effectively treat sleep apnea. There is nothing wrong with using sleep apnea equipment. Not everyone’s sleep apnea is related to nutritional or dietary habits, but a person with sleep apnea whose body mass index is greater than 30, who is using alcohol and who is not exercising owes it to their well-being to address these issues. The goal is eliminating, or reducing, the burden of sleep apnea.
- Diet and weight loss.
- 15 minutes of exercise daily.
- Discontinue tobacco.
- Discontinue alcohol.
- Good sleep hygiene.
Robert H. Kelly, MD FACP
HIP SURGERY, ANESTHESIA, AND DELIRIUM
In persons older than 80, delirium after surgery is too common. Delirium is when there is confusion and the ability to attend and remain oriented in the environment in lost or severely impaired for a period of time. With recovery from the trauma, pain, and immobility of surgery, postoperative delirium will resolve. Delirium is a marker of injury and a prognostic sign of potential increased risk of dementia in the future. Whether delirium is the cause of that increased risk or another sign of underlying impairment already present is not known.
A study was done of 940 patients in China who had suffered a fall with hip fracture. The patients were randomly assigned to receive either general or regional anesthesia. Was there a difference in the rate of delirium?
In the regional anesthesia group, (spinal anesthetic, nerve block, and sedation), 6.2% developed delirium, whereas in the general anesthesia group, 5.1% developed delirium. Length of hospitalization was the same. Death was more common in the regional anesthesia group (8 compared to only 4 in the general anesthesia group). Other researchers have also shown that general anesthesia is reasonably safe compared to regional anesthesia.
The best course of action for a person who has suffered injury and requires surgical repair is to follow the recommendations of the surgical team. It is prudent for that team to use tools, including the anesthetic approach, that they are most familiar with and are convinced are most beneficial for their patients. If the recommendation is for general anesthesia, you can be confident that it will not worsen the risk for delirium as you Recover.
Robert H. Kelly, MD FACP
NARCOTICS - MORE BAD NEWS
The CDC reports changes in narcotic pain use in the United States. Regulatory agencies and medical societies have urged reduction in opioid prescribing. Prescription narcotics were responsible for one-third of the 100,000 narcotic drug overdose deaths in 2021.
A CDC study looked at emergency department narcotic prescriptions. Narcotic prescriptions increased from 19% to 21% from 2006 through 2011. Reversing the trend, from 2011 to 2016, narcotic prescriptions decreased to 15% of emergency department visits. The new CDC study showed that narcotic prescription at the hospital for headache and migraine reduced by 98% and for back pain have fallen by 50%. In 2012, the CDC and the American College of Physicians published a policy that include a recommendation against routine prescribing of narcotics for back pain and migraine. Apparently, it was possible to reduce narcotic use by 98% when it comes to relieving back pain. There is this great experiment ongoing where what used to be right (narcotics for common pain complaints) has now been shown to have probably been 98% wrong.
Robert H. Kelly, MD FACP
PRIVATE CAREGIVERS: SIMPLE IS BEST
Does reporting improve home care by private caregivers? We know that in-home caregivers (who are not nurses) can help the frail elderly remain at home successfully. We know such care can be a boon for the family. Private home-based care is generally not covered by Medicare but is provided by families for their loved ones. “Right At Home” is a national home care provider with many franchise offices. The researchers at Harvard collaborated with the company to randomly assign franchises to an enhanced monitoring program designed to report changes in condition or to continued non-reporting status. Generally speaking, our caregivers do not report changes in condition to doctors or hospitals. They work with the family in many ways to help the patient, and the family decides when to call. In this research, a cell phone-based app was introduced into different franchises at separate times. The app would call upon the caregiver to report to the office changes in condition by responding to specific queries on the screen or keypad.
The intervention was called “Home Care To Improve Health Outcomes,” or “In-Home.” It was based on the idea that by introducing additional software and reporting, home caregivers could reduce the rate of hospitalization or death. The experiment ran from 2015 to 2018 and involved 269 franchises. 738,000 person months and 103,535 individuals. Across all regions, there was no difference in emergency room visits, hospitalizations, or rates of death with the In-Home program. There was, however, an increase in cost and time required by caregivers to do their work. The extra cost was, of course, paid in hourly wages by the families.
The authors write: “Our randomized evaluation of the In-Home Intervention found no impact on the primary outcome nor evidence of impact on hospitalization, ED visits, or mortality.” The authors go on to say that even when they “focused on subgroups in which we thought engagement might be stronger and better, there was no difference.” In other words, even cherry picking the groups they thought would benefit, they found no benefit of increased complexity in ordinary care. We’ll keep it simple for now. Mandatory reporting had no value.
Allan R. Kelly, MD FACP
QUOTES
“Julia didn’t like the way the news was delivered, by a doctor she didn’t know well. The doctor left the door open as she spoke to us. The doctor didn’t even sit down. So, I was upset this morning.”
Adeline Goss, M.D, 2022
“Throughout medicine, patients and clinicians alike are feeling the absence of robust therapeutic relationships.”
Caleb Gardner, M.D., 2020
“With every clinical encounter, it became clear that my goals for providing the best patient care and my goals for looking good were completely misaligned. What people really need is a doctor who can look at them, not the screen, to figure out what's actually going on.”
Lisa Rosenbaum, M.D., 2022
IMPORTANT CHANGE
Nurse Practitioner Claire Kelly-Legler is moving to Tulsa, Oklahoma with her family, and she will no longer be working in our clinic. We are excited for her new chapter in life and wish her all the best in her future endeavors.
PMH STORY
The PMH patient had never married and had no children. She had one brother who lived in Virginia. There were nieces and nephews, but none in Texas.
Growing old, dementia set in. She was increasingly frail. Serious medical problems indicated short life expectancy. The patient was no longer able to make her own decisions, and her brother, working with a PMH physician, made arrangements for hospice care. The goal was to create a more peaceful environment and to reduce or avoid trips to the emergency room. Trips to the hospital are often disruptive and anxiety-provoking, especially for those with dementia.
Near Christmas, the PMH physician recognized that the woman had had a change for the worse. Pneumonia was diagnosed from a chest x-ray and laboratory. Pneumonia in a patient like this is high-risk, and so the doctor went to her bedside to evaluate what was needed.
At the bedside, the woman was profoundly weak and unlikely to live long. The doctor called the brother, gave a report, and explained the situation. The woman was still able to open her eyes and say hello, and even said to the physician, “You’re my doctor, aren’t you?” During the phone call, the doctor asked if the brother would like to see his sister and talk to her. He said yes, and we switched to Facetime. The doctor held the phone so that the woman could see her brother. There was recognition, and the brother spoke to her. We all three visited. It was clear that the sister was comfortable, though weak, and the brother had the comfort of seeing her. After meeting with hospice and the nursing home team, the PMH doctor was about to leave the facility when a group of students from TCU came in with holiday cards for the residents at the nursing home. The PMH doctor asked if they would like to give the cards away individually, and a young woman said yes. The doctor said, “Would one of you like to give a card to the patient I just visited?” The student handed the card to her and they greeted each other with smiles, hello, and Merry Christmas. The card and visit by the student clearly brought the patient pleasure.
PMH is about continuity of care and professionalism. These priorities are good for patients, families, doctors, and the community at large. PMH strives to create a practice where the doctor is not “too busy” and can take the time needed to help the patient.
Allan R. Kelly, MD, FACP
AMERICAN HEART ASSOCIATION: GOOD HEALTH HABITS
After several decades of improving cardiovascular disease mortality, progress has slowed. There may even be an upward trend in cardiovascular mortality (Rehm et al, JAMA, 2016). Medical treatment, fitness, nutrition, and nonuse of tobacco have been cornerstones of past and future success. The American Heart Association reviewed these cornerstones and made new recommendations in 2021. Compared to prior recommendations, the focus is on an overall heart-healthy diet and not specifying certain foods as good and others as bad. There is increased focus on heart-healthy diet early in life. Key doctor recommendations include:
- Vegetables and fruits, not meat and potatoes, should be the high-volume elements of diet.
- Plant-based food, fish and low-fat dairy products are beneficial.
- Avoid ultra-processed food.
- Minimize added sugars.
- Use little or no salt when preparing food.
- Extra virgin olive oil has health benefits.
A final recommendation from the AHA: “Patients should not start drinking alcohol if they have never consumed any. Patients who already drink alcohol should limit their intake. Alcohol intake at any level to improve cardiovascular health is not recommended.” The AHA joins the American Cancer society in emphasizing alcohol use as a risk factor for poor health.
The new guidelines recommend 20 minutes a day of exercise. This can take any form: walking, Pilates, floor exercises, stationary equipment, and others. The key is to get up and move at least 20 minutes, seven days a week to improve strength and mobility.
Robert H. Kelly, MD, FACP
KNEE ARTHRITIS
Knee arthritis is common and can be disruptive, causing people to have to go to the emergency room or be admitted to the hospital. What is the best way to help people when the knees start to give out, and what are the goals of therapy?
A good experiment by doctors at Brooke Army Medical Center in 2019 enrolled 150 male and female patients with severe knee pain from osteoarthritis. 75 were randomized to physical therapy, and 75 to steroid injections in the knee. After one year, the patients were compared.
There was no baseline difference in the two groups of patients. The same sort of patients were randomized to physical therapy as to injections. The injection group was allowed to have a maximum of four injections in the course of the year. Most patients had two to three injections during that one-year period. After one year, the patients were compared.
The outcomes measured included pain relief, overall costs, and surgeries. The results showed better pain relief and better outcomes with physical therapy as compared to injections with steroids. Surgery on the knee occurred only in the steroid group. There were no surgeries in the physical therapy group. Most people want to do well with their knees and most people don’t want to have to have surgery. According to this research on knee arthritis, physical therapy is more likely to get people what they want than steroid injections.
Allan R. Kelly, MD, FACP
ONE OR MULTIPLE DRUGS FOR HYPERTENSION
Researchers in Australia compared low-dose multidrug therapy versus standard dose therapy for control of hypertension. One group was started on a compounded pill, called a poly-pill, with approximately one-quarter of the ordinary starting dose of Metoprolol (a beta blocker), Irbesartan (angiotensin receptor blocker drug), Indapamide (thiazide diuretic), and Amlodipine (calcium channel blocker). Low doses of each were compounded into a single capsule. In the other treatment group, patients were started on standard and escalating doses of a single medication with the addition of a second medication if the first medicine at higher doses was inadequate.
600 persons were enrolled. Some were already on blood pressure treatment with a single agent. None were at their desired goal blood pressure of less than 140/90. Blood pressure control was reassessed after 12 weeks and 12 months. Participants treated with the low-dose multidrug pill had significantly improved blood pressure control at 12 weeks compared with the volunteers treated more conventionally with higher doses of a single agent. Blood pressure control in the poly-pill group was also better at 12 months. Using a multi-drug low dose approach was more effective at achieving blood pressure control at 12 weeks and 12 months than was using higher doses of a single medication.
Robert H. Kelly, MD, FACP
PNEUMONIA: HOW LONG TO TREAT?
One of the great efforts of medical research is to define what is the preferred treatment. This question involves not only the selection of a drug or other treatment, but also the duration of treatment. The possibilities are vast.
We have previously written here about the duration of therapy for infection. We all remember the days of strep throat, where we were told to take all 10 days of penicillin, regardless of whether or not we were sick. Researchers in The Lancet 2021 looked at community-acquired (people living in their own homes who became ill) pneumonia requiring hospitalization. 310 patients, 18 years of age or older admitted to the hospital with pneumonia, were randomly assigned to two treatment groups. One group received three days of antibiotic therapy, followed by three days of placebo. The other group got six days of antibiotic therapy. Cure was defined as temperature of 100.4 or less, resolution or improvement in symptoms, and no additional antibiotic therapy for any cause, over 15 days of follow-up.
Seventy-seven percent of the patients in the three-day group and sixty-eight percent of patients in the six-day group were cured: cure was more common in the three-day group and less common in the six-day group. Adverse events were somewhat more common in the six-day group. This data supports reducing the duration of antibiotic exposure for patients treated in the hospital for community-acquired pneumonia.
One study is not enough to change the duration of therapy of important infectious disease problems like pneumonia, but we know now that shorter duration may work better than longer duration.
Allan R. Kelly, MD, FACP
STEPS PER DAY: FITNESS AND HEALTHY LIFE
In all settings, a program of physical activity (exercise), improves the quality of life and/or reduces adverse outcomes, including risk of death. A recent study looked at middle-aged adults and re-evaluated walking 7,000 steps per day.
The JAMA report found that men and women in the United States who walk or take at least 7,000 steps per day in middle adulthood showed a lower risk of mortality. 7,000 is not a magic number but it has been widely used. In this study, a pedometer monitored the number of steps taken. This was a study of healthy young adults.
Participants were divided into three groups, less than 7,000 steps, 7,000 to 10,000 steps, and more than 10,000 steps. Smoking history, body mass, alcohol use, healthy diet, and diabetes were all controlled. Approximately 2,000 subjects were studied with examinations and follow-up over the course of at least five years. 71% of patients were followed for 30 years!
Mortality risk was nearly 70% lower in the group with more than 7,000 steps compared to the group of less than 7,000. Higher number of steps (more than 10,000) was not better than 7,000. This is consistent with prior studies which have also shown the benefit of moderate exercise (more than 7,000 steps) compared to sedentary lifestyle (less than 7,000 steps).
If you are living a sedentary life and feel like you are not getting much exercise, get a pedometer and see just how many steps you are taking a day. They are available for less than $50. The pedometer empowers individuals to understand their own health. And if you find that you fall into the sedentary group and are taking less than 7,000 steps per day, then “steps” should be taken to avoid the low fitness category.
Robert H. Kelly, MD, FACP
QUOTES
“I greatly admired the style of my father’s death, putting aside the oxygen tent, and the similar decision of Uncle Will to die when it was time, without trying to eke out any extra days. When their deaths seemed to them inevitable, they simply died. Their acceptance was stamped with dignity, a quiet conscience, a sense of fitness.”
Charles Mayo, MD, 1968
“I knew, and know, that our system of not-care for the sick and scared is broken.”
Jessica Gregg, MD, 2022
“The glory of medicine is that it is constantly moving forward, that there is always more to Learn.”
William Mayo, MD, 1928
PMH STORY
COVID has caused changes, but the old lessons are still good. I recently visited a PMH member in long-term care. Because of covid, the doors were all locked. Knocking on the door for several minutes, calling the phone number, leaving a message, pressing the various buttons that were available to be pressed were all ineffective, and the door remained locked. Through the door window, I could see a few residents gathering in the dining room for supper. Everyone was busy. A man living at the facility could see I was at the front door and needed to get in. He came in his motorized wheelchair to the door. I noticed his hat: Korean and Vietnam vet. He unlocked the door, and I was able to enter, visit, and provide care to the PMH member that was at the facility.
On the way out, I stopped at the table where the man in the wheelchair was with two other men. I thanked him again for his help. We talked a little bit about football games. I told him that the important game that weekend was on Sunday: The Pee Wee Baseball Team Seawolves play the Yard Ducks. (I have a grandson on the Seawolves) Prior to parting, I thanked him for helping me. As I left the facility, I saw 15 newspapers piled up outside the front door. The door was about to close behind me (I did not want that to happen), so I quickly grabbed the door and, one armful at a time, I got all the papers moved indoors. The staff showed me where to leave them, and then I was on my way.
This time together with the other residents, who were not my patients, was possible because I was not too busy. I had time to pay attention and enjoy the fellowship. PMH changes my day for the better.
Robert H. Kelly, MD, FACP
FLU VACCINE REDUCES RISK OF DEATH FOR HEART PATIENTS
We are accustomed to getting our flu vaccine, and we know the vaccine prevents illness and death even in healthy people. We have been told the flu shot makes a difference, helps us to avoid hospitalization, and reduces the risk of wintertime death. So, placebo- controlled trials of flu shots are difficult.
Researchers in Sweden randomized 2571 volunteers who were admitted to a hospital with heart attack.They were recruited from 2016 to February 2020. The average age was 60, and 82% were male. None of the participants had had a flu vaccine for that year prior to the myocardial infarction. Half of the volunteers received a flu vaccine before hospital discharge. The other half got a placebo.
During three years of follow-up, all cause death rate was 41% lower in the influenza vaccine group compared to the saline placebo group. The author of the study, Dr. Frobert, was quoted: “Patients with cardiovascular disease should get their annual flu shot…a flu shot could prevent cardiovascular death…”
There is general acknowledgement that flu shots are prudent. It is remarkable to see a placebo-controlled flu vaccine experiment. But a 41% reduction in death rates in persons with recent heart attack is surprising. Whether this result could be the same in the United States, we don’t know. The experiment shows that an annual flu vaccine for our patients with vascular disease will likely save lives.
Allan R. Kelly, MD, FACP
COFFEE AND DEMENTIA
A study on coffee and green tea was done by internists and rehabilitation specialists and published in the Journal of the American Geriatric Society in 2021. Participants were 13,757 community dwelling individuals 40 to 74 years old. A questionnaire, completed between 2011 and 2013, measured consumption of coffee and green tea. The researchers asked whether coffee or tea consumption could influence the development of dementia.
The results: participants with higher coffee consumption had significantly lower risk of developing dementia. The total quantity of coffee consumption increased that level of protection. The authors report, “Coffee consumption of greater than three cups of coffee per day was associated with 50% reduction in dementia risk.” This was the first study I have seen looking at coffee and dementia. The association was more robust in men than in women. The risk of dementia in men drinking greater than three cups of coffee per day was cut by 80%.
Coffee is a complex biological preparation which includes not just caffeine, but many other phytochemicals. Observational studies do not prove cause and effect, simply association. Nevertheless, it is another sign and a reminder that not all habits are bad.
Allan R. Kelly, MD, FACP
OPIATE SAFETY: IS OLDER SAFER?
Humans have used opium for thousands of years. Opioids, unlike opiates, are manufactured molecules and do not naturally occur. Opium contains many opiates, and the most prominent are morphine and codeine, which make up approximately 80% of the opiates found in opium. Since the introduction of the opioid heroin early in the 20 th century, the opioids have competed with the opiates for relief of pain but there have been few, if any, head-to-head randomized control trials comparing opiates (morphine and codeine) with the opioids (such as heroin, oxycodone, hydrocodone, and tramadol). Researchers in Barcelona, Spain compared codeine and tramadol. Tramadol is a synthetic low potency opioid. Both codeine and tramadol are narcotics used for pain. This was an observational study, so it lacks the reliability of a placebo double-blinded controlled study.
The study looked at prescriptions for tramadol and codeine from 2007 to 2017. The researchers studied both death rates and adverse events in the two groups. Patients prescribed tramadol were twice as likely to die during the period of observation. Specifically, the death rate was 5.6 per 1000 years of use in the codeine group, but 13 deaths per 1000 patient years in the tramadol group. Other adverse events included fractures and cardiovascular events. These adverse events were higher in the tramadol group compared to the codeine group.
Another observational study has shown increase in mortality in patients with osteoarthritis given prescriptions for tramadol compared to patients treated with other drugs. So, we are being more cautious with tramadol and other narcotics. Increasingly there is data showing that the older opiates are safer than the newer opioids.
There are excellent alternatives to opiates for pain control. But there will be times in a person’s life when an opiate will be helpful, and a great relief to the patient and to the patient’s family. People have used opiates such as codeine and morphine for many thousands of years. In this research, codeine appears to be a better choice for safety and efficacy compared to tramadol, which was licensed in 1995.
Robert H. Kelly, MD, FACP and Allan R. Kelly, MD, FACP
IS THERE A BETTER TIME OF DAY TO TAKE BLOOD PRESSURE MEDICINE?
A randomized study of 19,000 patients in Spain looked at the timing of blood pressure medications. Half were told to take all blood pressure medicine in the morning. Half were told to take all the blood pressure medicine in the evening. At follow-up appointments, the advice was repeated. After 6 years, the researchers compared the risk of cardiac events or stroke in the two groups.
Adverse outcomes over the course of six years were 50% lower when taking blood pressure medicines at nighttime. The 6-year risk of a vascular event was 12% in the morning group and only 6% in the evening group. Blood pressure measurement in the nighttime group were 3 mmHg lower. However, a 3 mm reduction in blood pressure alone does not explain the 43% improvement in outcomes reported. But critics point out the trial design was potentially biased as prior studies have not established superiority of nocturnal dosing.
We await confirmatory studies to make a general recommendation. The Spanish researchers have challenged common medical practice, and we are paying attention.
Robert H. Kelly, MD, FACP
ANKLE ARTHRITIS: PRP
Ankle osteoarthritis is common, affecting 3% to 4% of adults. Dutch researchers compared platelet rich plasma (PRP) ankle injection to routine care in people with osteoarthritis. PRP is derived from a person’s own blood. The effect of the blood product when injected into the ankle was theorized to promote healing and pain relief. One hundred patients were randomly assigned either to a PRP injection or placebo injection. Average age was 56. The American Orthopedic Foot and Ankle Society Symptoms Score (AOFAS) was used, and a higher score means better function and less pain. PRP or placebo injections were given every 6 weeks for 2 injections. On the AOFAS, the PRP injection group improved from 63 to 73, whereas the placebo group improved from 64 to 75. PRP failed to improve ankle symptoms more than a placebo injection.
The benefits of PRP injections to date have not demonstrated benefits in controlled trials, but research continues.
Robert H. Kelly, MD, FACP
QUOTES
“The only one who knits my care together into a coherent whole is my 76-year-old primary care physician…we are more than a collection of our parts and need a new generation of doctors to see us as whole people and treat us that way.”
Richard Hencke, M.D., 2022
“Focusing on the patient: it is why we choose to become physicians…if I could spend my time with my patients and not all the hassles of documentation, billing, pre- authorizations and quality metrics, I would be a much happier physician!”
Linda Siy, M.D., 2018
“In the transition to electronic medical records, mandated through legal maneuvers and encouraged through financial incentives, clinical comprehension has been compromised.”
Mark Rosenberg, M.D., 2021
“We should all be so lucky to work at something we love until the day we die.”
May Owen, M.D., 1968
“The reward for work well done is the opportunity to do more.”
Jonas Salk, M.D., 1952
PMH STORY
The new PMH patient was well-known to the PMH doctor. He had cared for the patient’s wife for years, until she died from complications of chronic illness. The husband had not been ill, and with the death of his chronically ill wife, he decided to discontinue his PMH subscription.
Five years later, he called and asked if it would be possible to return to Dr. Kelly’s practice. He was not dissatisfied with his doctor, but he wanted to work with Dr. Kelly and felt like the PMH office would be better for him. We all knew this man. He had taken good care of his wife. We looked forward to seeing him again.
The staff greeted him as he came through the door. He was as happy to see us as we were to see him. Examination quickly showed that he had early dementia, confirmed in our subsequent workup.
So, our patient had been struggling with loss of his own confidence, his own ability to take care of himself, and, of course, the loss of his wife. Even at his first visit, he said to the doctor and the nurse how good it was to be back. We know how important understanding, familiarity, and responsibility are to all of us.
The PMH model emphasizes continuity of care. The PMH model also emphasizes comfort and convenience, our commitment to understanding our patients, their feelings, their needs and, of course, above all, the diagnosis, treatment, and prognosis of illness. PMH cannot provide everything a patient needs. There are consultants, hospitals, facilities and so much more. But for our patients, it starts with going to see the doctor, asking the doctor for help, and being respected and supported throughout their illness. We know that such support and care is found in offices and hospitals throughout our community. We are grateful to all of our colleagues for their care and understanding of their patients.
But for the gentleman who returned, now facing his own need, the PMH medical home gave him comfort, convenience, and the confidence that his needs would be met.
Allan R. Kelly, MD, FACP
PMH STORY
The patient was ill and had seen their urologist at intervals for months. A complication had arisen, and acute illness led the surgeon to send the patient to a hospital where Dr. Kelly relies on the hospital team for emergency care. There had been a prior diagnosis of prostate enlargement and several infections had occurred. Another infection was suspected, and he was admitted.
The next morning the patient’s daughter called Dr. Kelly. She was worried about lack of progress and that her father had had nothing to eat. Dr. Kelly was able to go to the hospital. He visited with the patient and family, examined the prostate and bladder, studied the information in electronic records, spoke with the nurses, and identified a probable obstruction caused by prostate cancer that required treatment. Arrangements were made for transfer to a different hospital where the patient’s urologic surgery team could address these issues immediately.
There is much in medicine today that seems administrative, perhaps even bureaucratic. It is hard to automate the complicated question of understanding a patient’s disease, understanding their needs, addressing their concerns, and, as the daughter put it, make progress. This is what PMH provided to the family. A call led to rapid assistance and cooperation with the rest of the team. But who does the family call? In PMH, everyone will know who to call.
Robert H. Kelly, MD FACP
MALARIA AND HUMAN VOLUNTEERS AT WALTER REED ARMY HOSPITAL
In the 19th century, research in the understanding of infectious diseases used human volunteers. The great pioneers of infectious disease, such as Louis Pasteur and Robert Koch, had their volunteers (often their own research assistants) exposed to microorganisms to prove that the microorganisms caused disease! Despite danger, people will still volunteer to undergo infection with microorganisms in order to learn more.
At Walter Reed Hospital, doctors recruited 25 volunteers in 2020. The research was to see if monoclonal antibodies administered before exposure could prevent infection with malaria parasites. The protocol called for infection of the participants with malaria by mosquitos. The forearm of the volunteers would be put in a closed space with infected mosquitos. Multiple bites would occur. 17 volunteers received monoclonal antibodies in various doses. 8 volunteers received no such monoclonal antibodies.
All of the 8 unprotected volunteers developed malaria parasitemia: they were infected. They were immediately treated. No serious illnesses developed. In the 17 volunteers who received the monoclonal antibodies, none developed malaria, even at the lowest dose of monoclonal antibody administered, and the antibodies were effective for up to nine months after infusion.
This experiment is a combination of the very old and the very new. What we do today is informed and guided by the giants in our past and the human experiments of today. Monoclonal antibodies play such a large role in our fight against the COVID virus. We see here that targeted monoclonal antibodies protect people from malaria. There are, of course, older ways to protect ourselves from malaria. Quinine and its derivatives, for example. But there will be situations where an intravenous antibody would be better. This is a breakthrough in what it says about monoclonal antibodies, and what it tells us about the hope for a malaria vaccine as well.
Allan R. Kelly, MD FACP
POSTMENOPAUSAL LASER TREATMENTS
Medical technology and procedures do not require the same approval process as drugs. For technology, safety is the key, and proof of efficacy is not required for technology licensing in the United States.
It can take a long time to complete a randomized control trial to help doctors determine whether the new technology is actually useful. In the meantime, the promise of the technology can go forward, and doctors who, based on testimonials, believe in the therapy, may recommend it to their patients.
Medical progress relies on randomized placebo control trials. So, it was good to see a publication from Australia in JAMA looking at fractional carbon dioxide laser therapies; (unfortunately branded as “Mona Lisa” treatments), versus sham treatments for postmenopausal vaginal symptoms.
The trial looked at multiple outcomes, including comfort, infections, and bleeding. Ninety women were randomized, half receiving the laser therapies, and half receiving a sham therapy, using the same equipment and the same experience, but delivering no laser treatment to the vaginal mucosa.
The article by Li, et al, concluded: “Among women with postmenopausal vaginal symptoms, treatment with fractional carbon dioxide laser versus sham treatment did not improve vaginal symptoms after 12 months.” There was no benefit of the laser treatment (compared with no laser) in any of the outcomes.
There was no meaningful improvement compared to a sham or pretended treatment. The average cost of laser treatments is $400 per visit. But with no definable benefit experimentally, laser is probably not a good choice. That a technology is available does not prove it is any good.
Allan R. Kelly, MD, FACP
PRP/PLASMA INJECTIONS FOR TENDONITIS
An experiment in England reported in 2021 randomized 240 patients with Achilles’ tendonitis into two groups. One group received platelet-rich plasma injection (PRP injection) and the other group placement of a dry needle without any injection (sham). Results of this PRP vs. sham were then analyzed.
Pain and function score was used to compare the two groups. Patients were followed up six months after treatment. Most patients improved regardless of the treatment. But pain scores were a little bit better in the sham group, though not statistically significant. Since a needle was used in both groups, there was no difference in complications between the two groups.
PRP, like stem cell treatments, is receiving a lot of attention. This study looking at Achilles tendinopathy did not show a benefit of PRP injection.
Use of topical treatments, simple oral analgesics, physical therapy, change in shoes, stretching, home exercise program, and time are effective and remain the best approach to the common care of musculoskeletal conditions. Plasma injections are apparently not worth the time, money, and trouble.
Robert H. Kelly, MD FACP
LIFE’S SIMPLE 7
Non-alcoholic fatty liver disease (NAFLD) is increasing and is the leading cause of cirrhosis. NAFLD is generally related to obesity. But the overlap of NAFLD and cardiovascular disease is notable. The most common cause of death in patents with NAFLD is cardiovascular disease.
The American Heart Association uses a new phrase “Life’s Simple 7.” It is probably Life’s oversimplified 7 but it does reflect the thinking of the American Heart Association, the Multi-Ethnic Study of Atherosclerosis group, and doctors generally. Here are the Healthy 7, all of which you will recognize:
- Healthy diet (less is more!)
- Regular physical activity, 75 to 115 minutes per week
- Normal body mass index, 23-27
- Not smoking (don’t smoke at all)
- Blood pressure, systolic <130
- Blood sugar, less than 125
- Total cholesterol, less than 200
There was a correlation between these healthy habits and the frequency of non- alcoholic fatty liver disease and cardiovascular disease. The phrase “Life’s Simple 7” is worth remembering.
Robert H. Kelly, MD FACP
QUOTES
“Of everything I’ve learned in medical school thus far, my favorite realization has been that I love people.”
Rachel Felix, medical student, 2021
“I had the good fortune of reconnecting [with my patient in the hospital]. We started right where we left off and it felt incredible. It felt like I had come home.”
Ryan Chippendale, MD, 2021
“Increasingly, evidence indicates that the electronic health record is imposing an intolerable burden on clinicians and may be degrading, rather than elevating, clinical care.”
Edward Melnick, MD, 2020
“We have to ask ourselves whether medicine is to remain a humanitarian and respected profession or a new but depersonalized science in the service of prolonging life rather than diminishing human suffering”
Elisabeth Kubler-Ross, MD, 1969
PMH STORY
The subscriber had spent the last six weeks in a nursing home. This nursing home
used a medical director system: Physicians were paid and contracted to provide the
resident’s care. The nursing home did not accept orders from outside doctors.
The PMH doctor came to see his resident. He had seen her several times before and
had a good relationship with the medical director. During this visit, a nurse came in the
room and reported a fall two weeks previously, sliding to the floor. She felt that the
patient was trying to move too much trying to get out of the chair. The medical director
had started routine Xanax. The nurse said the Xanax was not strong enough, and we
needed to increase the dose.
As the PMH doctor listened to the nurse, he noticed the resident getting a look over her
face, staring out the window, no longer engaged. When the nurse left the room, the
PMH doctor shut the door and listened to the resident: she reported that the staff were
not listening to her and were not being helpful. She wanted to go home.
The family had provided a sitter to be with her during daytime hours. The patient was
sitting in a wheelchair, and the PMH doctor then said, “Let’s explore.”
They went down two long hallways checking out the facility, greeting the nurses and
going to the Nurses’ Station. They then went out to a patio. “Oh, I haven’t been here.”
When on the patio, she met another resident, a man that she had known for years, who
was sitting there with his son. Her joy and liveliness were a breath of fresh air. The son
of the man said, “I knew her before she came here, and she is such a wonderful
Person.”
The PMH doctor encouraged the caregiver to take the patient out of the room several
times every day to explore, move, and to give her mobility that she does not have any
more in her own legs. Dr. Kelly contacted the medical director and reported “the Xanax
isn’t working: The nurses say she is getting no better at all,” and gave the doctor the
report on the travels about the nursing home and plans to help the patient with her
desire for more mobility and activity.
The PMH doctor had time to listen and explore. With PMH, the doctor has the time to
understand better the problems faced by the nurses, the caregivers, the resident, and
the doctors.
Allan R. Kelly, MD FACP
COST OF CARE
William C. Roberts has been an internist and a leader at Baylor University Medical
Center in Dallas for decades. He writes about medical costs in a recent BUMC
Proceeding essay.
His review of the cost of a cesarean section looked at charges at Memorial Medical
Center in Modesto, California. This is a large hospital, busy with cesarean sections.
The charges for routine cesarean sections with brief hospitalizations ranged from $6000
to $60,000, and the cost appeared to be determined by the insurance plan of the
patient. Dr. Roberts tells the story of his own family: “One of my granddaughters
recently had a C-section and rather than paying the higher cost using her private
insurance, she and her husband paid the smaller price by paying cash. Money tends to
lose meaning when it is connected to medicine.”
In our office we also see examples. This summer a patient called from x-ray. His co-
pay for his insurance for a CT scan of the abdomen was to be $2500. He hesitated to
make such a large payment because he didn’t really know what a CT scan might cost.
We quickly called Envision Radiology to check on their cash price: $595. We told the
patient his choices, and he went for the cash price.
We see this with medications as well. The difference in price can be not only a factor of
10, but a factor of 100. Nobody wants to spend $100 when they can get the same care
for $1.
We continue to study this problem. We encourage our patients to look into the costs,
and to shop for a better price. That is true for our office as well. If you need our help,
just call and we will see what we can do to find out your options.
Allan R. Kelly, MD FACP
STATINS AND ELDERLY AMERICANS
Ever since evolution of statin therapy to reduce cardiovascular mortality, there has been
uncertainty about statin benefits for the elderly. All the early statin prevention trials
focused on younger people, even as young as 40.
For decades, the American Heart Association and other organizations advised that they
could not endorse the use to statins in adults over the age of 75 or 80 because of
limited information. Over the past 10 to 20 years, adults aged 80’s and 90’s, had
doctors recommend discontinuation of statins.
There are two areas of research that may change that approach. First, the VA Medical
Center published data in JAMA looking at adults over the age of 75-90, and how statin
use affected death and serious adverse cardiac events. The study looked at veterans
who had no history of atherosclerotic disease and no past or present use of statins in
their VA charts. Then they studied healthy veterans who were initiated on statins and
compared their outcomes to healthy veterans who were not initiated on statins. This is
an observational study, and prone to confounding. But the results are important.
Healthy veterans started on statins after age 75 had a 20- 25% reduction in overall
mortality during the 7 years of the study. The data held for women as well as men.
Reductions in cardiovascular death alone could not account for larger reductions in
overall death.
Second, Baylor Scott & White is leading a randomized control study, the
PREVENTABLE Trial to understand this even better. They will randomize adults over
age 75 who are in good health and who have no heart disease, dementia, or disability,
to statin or placebo. They will follow participants for five years, testing cognitive and
physical ability, and monitoring for major adverse cardiac events as well as all causes of
death. If you are interested in volunteering, call 1-888-507-3732.
Allan R. Kelly, MD FACP
MEDICINE PRICES AND PMH
Pricing is unpredictable even for common problems. [For example, post-menopausal
symptoms are common.] Treatments include oral estrogens, topical estrogens,
transdermal estrogens, and selective serotonin reuptake inhibitors.
Plain estrogen or Estradiol is available as a generic pill. At Good RX, the cost was $0.90
per month. Topical estrogen Imvexxy cost $572 per month. There is something odd
about a situation where medical treatment (estrogen) can be purchased for either
$572.00 per month or $0.90 per month.
In the non-estrogen category of post-menopausal treatment, there was only one drug
approved by the FDA. Paroxetine, also called Paxil, was approved by the FDA to treat
menopausal symptoms at a dose of 7.5 mg. The monthly cost on the 7.5 mg pill is
between $150.00 and $211.00. But if one were to purchase a 30 mg Paxil tablet and
just take a quarter of a pill (or ask a pharmacy to make an 8 mg capsule) the cost would
also be less than $1.00 per month. The FDA-approved product costs $211.00 and the
simple modified available product costs less than $3.00 per month.
When faced with medication cost that we find burdensome, there will often be an option.
The option may not be an FDA-approved form of a product. Cutting the pill or having a
pharmacy compound a capsule can save a lot of money. With ingenuity, we can control
Costs.
Robert H. Kelly, MD FACP
GENERAL VERSUS REGIONAL ANESTHESIA
A recent report compared dementia risks from general anesthesia (GA) versus a
regional anesthesia (RA) for matched surgeries in Ontario 2007 to 2011. The patients
were followed for about five years after the procedure. General anesthesia involved
both inhalation and intravenous anesthetic agents. Community-dwelling older adults
without dementia and at least 66 years old underwent one of five surgical procedures:
hip surgery, hernia surgery, knee surgery, hysterectomy, and prostate surgery. A total
of 41,000 divided between general GA and RA. The preoperative risk measurement
was slightly higher in the RA group suggesting a higher frequency of emergency
surgeries. However, high risk issues such as head trauma, stroke, and diabetes were
more common in the GA group.
Over the course of five years approximately 6% of patients in both groups developed
dementia. Previous studies had shown an incidence of dementia on the order of 23%
and this increase in the overall risk of dementia was noted in both anesthetic groups.
GA did not increase dementia risk.
Postoperative delirium was a problem especially in those who used alcohol
preoperatively. It is best to discontinue all alcohol and all smoking at least two weeks
before surgery. But long-term cognitive effects appear low.
Surgeries studied here are low-risk surgeries. High-risk surgeries, such as heart
surgery and brain surgery, are more likely to be associated with confusion or delirium,
not because of the anesthetic, but because of the underlying disease processes.
Robert H. Kelly, MD FACP
KETOGENIC DIET AND COGNITION
An experiment was done in 50 to 90-year-old patients with Alzheimer’s disease. The
experiment revolved around reducing carbohydrates in the diet and pursuing a
ketogenic diet or a diet low in carbohydrates. Twenty-one patients were studied.
Performance and activities of daily living (the usual activities of life) were used as the
outcome variable. Compared with usual diet, patients on a high-fat, low-carbohydrate
diet had a distinct improvement in measured components of independence.
Cardiovascular measures were improved. There was mild increase in cholesterol,
although mostly of HDL “good” cholesterol. The study concluded after only two weeks.
In this trial, a low carbohydrate diet was better for the brain.
Robert H. Kelly, MD FACP
QUOTES
“I can tell you I’d rather have a doctor that understands my concerns and listens to me
than one who scored in the 99 th percentile in their standardized exams but never
questions the diagnosis.”
Ashley Brodrick, Medical Student, 2021
“All medical knowledge has a half-life. We no longer prescribe arsenic for syphilis or
milkweed for pleurisy: but we do need physicians with a curiosity and discipline to
continue their learning.”
Benjamin Doolittle, M.D., 2021
“The EHR, which was intended to improve patient care, has had the ironic and
unintended consequence of impairing practice efficiency largely because of poor
design, they focus on regulatory reporting and burden is placed on clinicians by data
Entry.”
Yumi DiAngi, 2017
“For many physicians, listening has become a luxury squeezed out by time constraints,
the demands of electronic health record and the countless metrics demanding our
attention. Somehow in our efforts to systemize all we know (and make it profitable), the
centrality of the doctor-patient relationship got lost.”
Lisa Rosenbaum, M.D., 2021
PMH STORY
A member who lives out in the country had been on vacation with her family. She had just not felt well. After vacation, she called the office, and was invited to come right over.
She did seem uncomfortable and was not in good spirits. Vital signs were normal. Abdominal examination was slightly abnormal but nothing specific. A couple of calls found a radiology office that could do a CT scan of her abdomen right away. Laboratory was obtained and the patient went a few blocks away for the x-ray. After the x-ray was completed, the radiologist immediately called Dr. Kelly to advise about the finding of a ruptured appendix with abscess. She returned to the office. A call to Harris was met with good coordination by the admissions office and she went directly to the hospital where consultation and plans were made for care of the appendicitis.
We were not too busy. We are well aware of the resources in the community. We care for patients across different levels of care, and the patient was admitted to the hospital within an hour and a half of coming to the office. She did well with treatment and recovered.
This would not have been possible for that patient if there was no PMH. At times PMH doctors will see their patients at the emergency room, for that is a good way of getting immediate care, rapid laboratory turnaround, and admission to the hospital. But with PMH it is good to know that there are alternatives, and it is good to know who will be taking care of you in the hospital. We think PMH helps both doctors and patients.
Robert H. Kelly, MD, FACP
VIRTUAL VISITS WORK WELL
Continuing attention to the benefit of virtual visits, JAMA Surgery reported on virtual versus in office post operative visits. Typically, after surgery a person will go in to see their surgeon for an in-office post-operative follow up. But now, visits can be done either virtually or in person. Would that be as good? This was looked at in the research.
Robert H. Kelly, MD, FACP
VACCINES: SUCCESS & FAILURE
We have cared for patients with life-threatening viral infections since going into medicine. The danger was dramatized in the 1980’s with the emergence of the HIV epidemic, and then in the 90’s the hepatitis C virus epidemic. Both of these epidemics have continued to kill many thousands of Americans every year. Fortunately, we have developed excellent antiviral therapies so that if diagnosed, the infected persons can be protected by medical therapies.
Allan R. Kelly, MD, FACP
OBESITY AND THE PREVENTION OF DIABETES MELLITUS
Dr. Joslin of Massachusetts was a great leader in understanding and treating diabetes. In JAMA in 1921, he wrote about his peaceful New England village where he had cared for seven persons who had severe diabetes. He noted in his article that six of the seven had died during the course of treatment, but one had survived. He went on to say that six of the seven suffered with obesity, and those were the six that died.
Allan R. Kelly, MD, FACP
EGGS: BETTER THAN WE EXPECTED
The authors studied approximately 500 articles about egg consumption published 1966 through 2020. During the same interval, there had been changing opinions about egg and cholesterol intake. For example, in 2000, the American Heart Association recommended that less than 1 egg per day be eaten, but when the guidelines were re-written during the interval 2015 to 2020, there were no specified limits on egg consumption. There had been no placebo-controlled trials. Prior studies had been inconclusive. This study combined all the data: median follow-up 12 years, 1.5 million cases and 150,000 cardiovascular events. The authors compared 3 levels of daily egg consumption: 0, 1, >1.
Robert H. Kelly, MD, FACP
DIABETES AND DEMENTIA
Dementia is a major problem for the elderly. Diabetes is an increasing problem for the country. Authors from the University of Paris writing in JAMA explored the association between diabetes and the risk for dementia.
Allan R. Kelly, MD, FACP
QUOTES
“The economic disruption caused by COVID-19 obliges clinicians to protect people from the financial stresses of needlessly being turned into a patient.”
Gilbert Welch, M.D., 2021
“Medicine was never intended to be like this. With all the political hand-waving and jargon about taking care of patients, the expansion of government and private insurance companies into healthcare has put all of our best intentions in jeopardy.”
-Marc Siegel, M.D., 2020
“Cultivate equally well your hearts and your heads…doctors are given over now days to science.”
William Osler, M.D., 1899
“If it were not for the great variability among individuals, medicine might as well be a science and not an art.”
William Osler, M.D., 1892
“That is the core of our job, to pull out a person’s humanity and let that light the way.”
Jessi Humphreys, M.D., 2021
PMH STORY
The patient's daughter called from California. Said she was worried about her mother and that she was afraid her dad would not call. Dr. Kelly knew that her mother was not well. After talking to the daughter, it seemed better to address the patient's needs at the hospital.
We are working more often with a hospital team. This means that other hospital doctors may be assigned to the case and help direct care. Dr. Kelly continues to visit, contribute to care, and play a role in the planning during hospitalization. This PMH story shows how the important role we play has not changed.
Visiting with the patient in the ER that first night, there was possible pneumonia on chest x- ray. Decision was made to proceed with admission and treatment. CT scan of the chest raised greater probability of viral infection. COVID testing was positive. Dr. Kelly returned the next morning around 7:00 to visit. The patient was stable. Plans were underway for admission and recommendations were left for modifications in care.
As Dr. Kelly was walking out of the emergency room, he pulled up the patient’s husband's number on his iPhone and dialed it. Out of the corner of his eye, behind his mask and face shield, Dr. Kelly saw the back of a man in a sports jacket in the waiting section of the emergency room. Dr. Kelly recognized the figure and realized that the man he saw was the person whose phone he was dialing.
Dr. Kelly went into the emergency room waiting area and visited with the patient’s husband, then returned to see the patient to give her the details of this conversation and her husband’s proximity and involvement. Hospital policy forbade the husband to visit her. Dr. Kelly asked the patient if she had any instructions. She told him to tell her husband to go home and to eat something. She worried about him as he is somewhat frail himself. Dr. Kelly passed the instructions on to her husband.
The patient's care progressed, and her needs were met. This would likely be true even if Dr. Kelly did not visit. What is important and what the hospital cannot provide is recognition out of the corner of the eye and the intuitive understanding of a patient's condition. PMH has its pros and cons, we recognize that. This episode is an example of how PMH helps.
Robert H. Kelly, MD, FACP
APPENDICITIS
Doctors in Finland continue studying antibiotic only (no surgery!) treatment of appendicitis. Laparoscopic removal of the appendix with short duration antibiotics causes little morbidity or mortality. It is hard to imagine how we can improve on the current surgical management of appendicitis. But over the past 10 years, researchers in Finland have shown that the overall complication rate is decreased in randomized trials where patients are randomized to medical treatment initially and not surgical treatment. If the patient did not recover quickly, surgery was performed. In their initial experiments, they used intravenous antibiotics, but in experiments reported this month in JAMA, surgical teams randomized patients to treatment with either IV or oral antibiotics, and surgery only if antibiotics failed.
In this recent trial, successful treatment without surgery was achieved in 70% of those treated with oral antibiotics, and 74% of those treated with IV antibiotics. There was no statistically significant difference between the oral and IV treatments. The possibility of treating appendicitis patients as outpatients without surgery is still not mainstream. But simplifying treatment and having less invasive options available for our patients and their families is progress.
This research was done by departments of surgery in Finland. Appendicitis is still a disease managed by surgeons. Even well established, standardized treatments can be challenged with new ideas.
Allan R. Kelly, MD, FACP
KNEE ARTHRITIS
Knee arthritis is a common problem. After age 60, approximately 37% of persons will complain of significant knee arthritis in surveys. As age increases, so does the incidence of arthritic knee pain. There has been a significant change in our approach to alleviating the pain and discomfort and limitations of knee osteoarthritis.
In the past, doctors would recommend steroid injections to the knee and oral medication such as Motrin, Aleve and even narcotics. The American Rheumatologic Association now identify the primary option for treatment to be topical nonsteroidal anti-inflammatory drugs. This option, like Voltaren gel, became available 14 years ago. In 2020, Voltaren gel, also called diclofenac, became available over the counter. Topical nonsteroidal drugs are equal to the effect of the oral nonsteroidal drugs. In other words, applying a topical nonsteroidal to the knee gives the same results as an oral nonsteroidal in randomized trials. But the oral nonsteroidals risk adverse effects, including ulcers, kidney disease, and increased cardiovascular risk. The new treatment with topical nonsteroidals is the better choice.
There are other interventions that we know will help. Exercise and weight loss are at the heart of making things better. Any type of exercise can work: Strengthening exercise, aerobic exercise, tai chi, physical therapy: All will statistically reduce the degree of pain.
Joint injections with steroids now are reported to have uncertain benefit. A single injection for a life event, such as a wedding or a trip, may make sense. But repeated injections increasingly are seen as more risk than benefit.
The most reliable nonsurgical interventions for knee arthritis are available without a doctor’s prescription: Topical diclofenac gel, daily exercise, weight loss, and tai chi. For those people who cannot get good results, and who are increasingly impaired, surgical treatment typically results in significant pain relief and increased mobility.
Allan R. Kelly, MD, FACP
REDUCING INFECTION RISK
Researchers from the University of Michigan tried to reduce operating room infection risk by increasing operating room sterile precautions. The basic approach for the past 100 years to reducing operating room risk is antiseptic preparation of the skin of the patient, and the OR team. The OR team puts on sterile gowns and gloves. After the patient is asleep, sterile drapes are placed over the patient to isolate the area where the incision will be made. Infection rates after a clean surgery are very low. But researchers asked whether clothing the patient in a sterile head covering and sterile gown before going into the OR would reduce infections.
The study looked at operative infection rates during three periods of time: Routine care, routine plus hair covering care, and routine plus hair covering and sterile surgical jacket. During a period of one year’s observation, there was no change in the surgical infection rate in the three groups. Commonsense, straightforward effective reduction of bacterial organisms coming into the operating room, did not improve protection provided by sterile skin preparation and aseptic precautions already in common use.
Postoperative infection is caused by bacteria on the skin of the person being operated on and bacteria on the surgical instruments and hands of the surgeon doing the operation. Preoperative head covering and sterile gowns on patients had no effect. Researchers will continue to try to find new ways to reduce our infection rate. But once you cut through the skin, bacteria are unavoidably introduced into a usually sterile part of the body.
Allan R. Kelly, MD, FACP
TELEHEALTH
Telehealth visits, both video and audio, have now been embraced by the medical community. Even Medicare is allowing visits with the doctor while you are in your own home. Availability for such visits has always been a part of PMH, but there is now a much wider acceptance of these visits. Recent reports have shown the value of these. In some ways, a telehealth visit on FaceTime, Doximity, or even just with a dedicated time for a phone call is the modern equivalent of a house call. Much of the information and knowledge that might be shared at a doctor’s office visit, or if the doctor came to the house, are shared on a telehealth visit.
A study in Boston showed 68% of patients would be satisfied with a telehealth visit. The study estimated that patient saved more than two hours of time from their schedule by using telehealth. This time would have been spent driving to and from the doctor’s office and waiting. Some of the telehealth visits were done with family providing the link. Telehealth visits with the patient and a loved one are often even more productive. Readiness of patients for telehealth visits has improved. In the Boston study, nearly half the patients had the technology to have a telehealth visit. In 2018, only 8% of eligible patients had the technology for a telehealth visit. In a separate study of patients who consented to the telehealth visit but did not complete one, only one-third actually went to the office for a face-to-face visit. The two-thirds who could not make it to the office were left without the help they wanted. Making telehealth work will help patients and their families.
Robert H. Kelly, MD, FACP
QUOTES
Doctors are only human, perhaps with more insight because from the very character of their work, they gain insight into human nature, and thus comes to understand it well and respect it highly.
-J.M.T. Finney, M.D., 1940
There are individuals - doctors and nurses, for example-whose very existence is a constant reminder of our frailties.
-William Osler, M.D., 1904
“I teach you that being a real doctor isn't a stamp on your diploma. You can't master it from a book…being a real doctor is being present and vulnerable. It's blurring the lines of physician and friend. Telling them to never give up hope while helping them to let go.”
-Rana Garris, M.D., 2020.
“Live long enough and eventually the body fails. It betrays us.”
-From the book titled Elderhood by Louise Aronson
FROM THE OFFICE OF DR. ROBERT KELLY
Martha Claire Kelly-Legler, Nurse Practitioner, will join Dr. Robert Kelly’s practice on 03/22/2021.
She graduated from University of Minnesota (Master of Nursing Science), St. Olaf (BA of Russian Language) and University of Texas Medical Branch in Galveston (Nurse Practitioner). Her clinical work has been at St. Cloud Hospital in Minnesota, Harris Hospital, and rotations at various medical practices here in Fort Worth. She spent approximately six months interning with Dr. Robert Kelly.
NP Kelly-Legler understands PMH and is in a position to be a resource and expert provider for PMH subscribers. She will provide care in the months and years ahead. Many of you will undoubtedly have a preference to see NP Legler instead of Dr. Kelly. This is understandable. However, there will be times when you may find yourself seeing one or the other because of needs that arise either in or out of the office. With two providers, we can better respond to urgent care needs.
In all cases, there is open and frequent collaboration between Dr. Robert Kelly, and NP Kelly-Legler. In all difficult and complex cases, there will be immediate collaboration until problems resolve.
This is a step-up for Dr. Kelly and our PMH office. This improves the ability of our office to do the work that we promise to do. We welcome NP Legler.
PMH STORY
The member had become ill, and the family was worried. An area of infection was suspected in the ear, not a simple ear infection. She had been to an emergency clinic and drops were started, but the area of inflammation seemed to be increasing. There was confusion and she came to the hospital.
Dr. Kelly saw her in the emergency room. There appeared to be an area of infection. Antibiotics were started and an infectious disease consultant suspected that infection was present and continued antibiotics. However, the appearance of the inflammation was atypical. It was the weekend but Dr. Kelly texted an ear, nose, and throat specialist. This specialist texted back saying that he would be by the next morning.
Dr. Kelly was seeing the member on rounds when the specialist arrived. Doctors do not see each other as much as they used to. So, it was good to see the ENT doctor appear and say good morning. Dr. Kelly and the specialist then went to the patient's room, a quick examination led to a decision to proceed with biopsy to confirm the diagnosis. The biopsy showed cancer. .
This is a PMH story about the importance of our medical community and colleagues. Collegiality is the spirit of cooperation, a synthesis of hard work that benefits a patient. Their value to a patient is great but it comes and goes rather quickly. Professionalism, continuity of care, collaboration has a different value when it extends over years and decades of life and of needing medical care. And that value is great. That is part of what PMH provides.
Robert H. Kelly, MD, PLLC
HEARING AIDS AND PERSONAL SOUND AMPLIFICATION PRODUCTS
All of us will lose hearing acuity as we get older. It is common to ask if a hearing aid can help. Hearing aids have been available only from otologists and physicians, and these hearing aids are expensive. There is a newer product called a personal sound amplification product. (PSAP) You can search this on the web and find devices that are inexpensive. We have no intention of replacing the judgment and guidance of our otology colleagues and hearing aid centers, but we thought you would be interested in a controlled study from Korea comparing hearing aids (expensive) and PSAPs (cheap).
Allan R. Kelly, MD, FACP
SOFT DRINKS MAY BE DANGEROUS
Researchers in Europe published a large, retrospective study regarding the association between soft drink consumption and increased risk of death. The study included more than 450,000 patients over 10 Western European countries. The participants reported their frequency of soft drink consumption and other lifestyle habits (degree of physical activity, smoking status, etc.). The researchers then followed the medical records of these patients for almost two decades, taking note of the cause of death. The results of the study found that people who drink at least two soft drinks daily were more likely to die younger than those who do not consume soft drinks. Consumption of artificial sweeteners was even worse. While many people believe that “diet” or low-calorie sodas are healthier, artificially-sweetened soft drinks were associated with an increased risk of death from cardiovascular diseases, such as heart attacks and strokes, than occurred in people drinking sugar-sweetened beverages.
Kaitlin Phillips, MS IV
WHAT MEDICAL NEWS INTERESTS PEOPLE?
The Journal of the American Medical Association keeps track of how many people come to their website and what articles they read. As of December 2019, the most popular article reviewed on-line in the JAMA network was on firefighters, pushups, and the development of cardiovascular disease. More than 500,000 Americans reviewed this study.
Allan R. Kelly, MD, FACP
TESTOSTERONE AND MALE AGING
At the University of Pennsylvania, 170 men were studied to see the effects of testosterone replacement on coronary artery calcification or plaque. Testosterone treatment was compared to a placebo and the volume of cholesterol plaque potentially blocking the coronary arteries was measured. The average age was 70.
Robert H. Kelly, MD FACP
SMOKING CESSATION
Tobacco use contributes to premature disability, illness and death, especially COPD and atherosclerosis. Its use reduces healthy survival as much as 20 years from expected. Tobacco use is also much more common in those with mental illness -- in my opinion, it causes mental illness. Stopping smoking will return a person to normal risk of cardiovascular disease within five years, and a normal risk of lung cancer in 15 years. Psychological health also improves. Getting off a toxic smoke improves vigor.
Robert H. Kelly, MD FACP
PMH QUOTATIONS
“Ask any physician of 20-year standing how he has become proficient in his art, and he will reply, by constant contact with disease: He will add that medicine he learned in the schools was totally different from the medicine he learned at the bedside… Having earned doctor of medicine, you have only reached a point from which you can begin a lifelong process of education.”
William Osler, M.D., 1903
"Amid the complexities and changes in healthcare today, Medicines' most fundamental element remains the relationship between patient and physician. Practicing physicians despair that the focus on cost has reduced them to cogs in the healthcare business machine, with daily reminders of ever-growing productivity expectations on top of questioning regulatory and clerical demands."
John Noseworthy, MD, 2019, President, Mayo Clinic
"[The Mayo Clinic] was built on two durable and influential principles. The best interest of the patient is the only interest to be considered, and, in order that the sick may have the benefit of advancing knowledge, union of forces is necessary."
William J. Mayo, 1910
PMH STORY
I met with a young hematologist. He is new to our town with good credentials. I look forward to working with him. He came to the office with an administrator from one of our top hospice groups.
They asked about PMH. I told them that one of the principles of PMH is continuity of care, and we continue to care for our patients who are on hospice. The doctor said, “Oh that is so good. It is so important for our patients. They often feel abandoned when they go onto hospice. It would make such a difference if their doctor continued to follow them.”
Despite this, his group had decided, as a general rule, that they will not follow their patients who transition to hospice care. The hospice administrator confirmed that 99% of doctors stop following their patients who go to hospice. At PMH we think that doctors help patients by providing continuity of care. It is not simply about feelings or personality. It is about quality of life, the care they receive, and the effectiveness of that care. It is about bringing knowledge, understanding and relationships to create something better. As the doctor and the administrator from the company acknowledged, there is something important about continuity of care.
We at PMH are committed to this principle: When our patients go on hospice, we will follow them and care for them and their families as long as we can be of value and service.
In the past month I have had three people die on hospice. We never stopped caring for them. The family never had to introduce themselves to a new doctor as their loved one was dying. Nor did they have to rely on doctors who did not know their loved one. We all know that there will be problems. The doctor will be temporarily unavailable or out of cell phone range. There will be interruptions even at PMH. But we make a commitment to continuity of care. Like patients, our colleagues know that this is good.
Allan R. Kelly, MD, FACP
CPAP: GOOD FOR PEOPLE WITH SYMPTOMS
Obstructive sleep apnea (OSA) has been around a long time. We know that when people fall asleep, their blood pressure, vital signs, and their breathing patterns change.
Allan R. Kelly, MD, FACP
DIET CHANGE CONTINUES TO SHOW PROMISE
We have all been learning how to change our diet to be healthier and avoid illness. The old days of steak and potatoes every night are long gone. The “Mediterranean Diet” has shown a reduction in the risk of cardiovascular events. The DASH, a sodium deprived diet, has shown statistical benefit compared to a controlled diet. A vegetarian diet has shown a reduction in risk, and, of course, low calorie diets have also reduced risk.
Allan R. Kelly, MD, FACP
SIMPLE MEASURES
Sometimes we are reminded that simple elements of healthcare may be as important as are the complex and expensive ways of healthcare.
Robert H. Kelly, MD, FACP
THE PREVALENCE OF VIRAL PATHOGENS VIRUSES IN HEALTHY PEOPLE
A study in 2017 was done at the Statue of Liberty in New York City. Healthy sightseers with no reported illness had viral testing done. The researchers collected nasal swab samples to see how many harbored viruses that can cause illness.
Robert H. Kelly, MD FACP
PMH QUOTATIONS
“If we could give every individual the right amount of nourishment and exercise, not too little and not too much, we would have found the safest way to health.”
Hippocrates, 301 BC
“Primary care practitioners must wade through EMR auto generated boiler plate pablum to figure out what consultants really thought about their patient.”
H. Gilbert Welch, M.D. 2020
“No greater opportunity or obligation can fall to the lot of a human being than to be a physician. In the care of the suffering, she needs technical skill, scientific knowledge and human understanding.”
Tinsley Harrison, M.D. 1950
“You survive in the new [medical care] system by giving the computer complete attention, the kind of attention we used to reserve for a patient. By default, the patient moves down to second place. As sad and horrifying as this sounds and feels, it is becoming the new reality.”
Elizabeth Toll, M.D. 2020
“Instead, take these patients’ preferences seriously as a way to respect them as persons and to protect their liberty. Physician’s reluctance to treat patients over their objections may therefore reflect a wellfounded moral intuition rather than mere self-interest or pragmatism.”
Mark Navin, Ph.D. 2019
“What we considered to be medical fact today may be medical fiction tomorrow.”
J. Willis Hurst, M.D. 2007
PMH STORY
A patient called. The young PMH member had gotten a tattoo at the base of his neck. He scratched a scab next to the tattoo and there was drainage of pus. He called his PMH doctor for advice on how to proceed.
There was no fever, chills, or vomiting. But the report of pain, redness and drainage was worrisome. It was on a weekend. The PMH office and laboratories were closed.
The description of the drainage was not typical for a common skin infection, likely related to this tattoo. Although a visit would likely have confirmed what the member was saying on the phone, the question in the doctor’s mind was the identity and resistance pattern of the organism causing the infection. It had come about after some instrumentation: the possibility of a health facility acquired infection, or resistant organism, was likely.
The member lived in Fort Worth—it would be easy enough to go to the Emergency Room to check a culture. Trips to the ER carry a burden of time, money, and inconvenience. Dr. Kelly was aware of a nearby Care Now clinic. He called the clinic and spoke with the Nurse Practitioner there. He requested a wound culture and to start antibiotic treatment. The Care Now clinic stated that this would not be a problem. Dr. Kelly’s patient was seen and treated. Empiric antibiotics were provided as recommended by Dr. Kelly. The patient followed up with Dr. Kelly, and the culture results were reviewed.
PMH doctors want to match the patient’s needs with the care given. To improve speed and convenience, visits like this can be handled at urgent care facilities. The outcome was favorable. This is the tailoring of care to a patient’s need which is not always available in large traditional clinic settings where nurses often process inquiries for emergency care. Today, we have many options, and we can make choices based on what is best for each patient.
Robert H. Kelly, MD FACP
LOW BACK PAIN AND OCCUPATIONAL INTERVENTIONS
Low back pain is common. For many patients, who have a normal exam and no neurological loss or impairment, research supports a simple approach based on time, activity, and Tylenol.
Allan R. Kelly, MD, FACP
MORTALITY RATES IN MEN AND WOMEN
Researchers from all over the United States reported on the effect of influenza vaccination on the elderly on hospitalization mortality. A graph was published in the Annals of Internal Medicine (2020:172:445-452), that showed male and female death rates between ages 60 and 70 per 10,000 persons. The study had its strengths and weaknesses, but the data on mortality rates was eye-opening to me. I have cared for men and women in the over 60 age group of course for a long time. But this figure reminded me that we have a problem that we don’t entirely understand.
Allan R. Kelly, MD, FACP
TELEMEDICINE
Dealing with the corona virus has opened our offices to the video conference. From the beginning, directness has been one of the 5 PMH key principles. Having a direct relationship, taking advantage of electronic communication, is important at PMH. We have initiated FaceTime videos and video conferences with patients when we make rounds in nursing homes. But during the COVID epidemic, the role of video conferencing has increased.
Allan R. Kelly, MD, FACP
COVID-19
As of May 12, 2020, in Tarrant County there were 3745 COVID diagnosis and 104 deaths, in a population of 2.08 million. Although not seen by the public, the impact on healthcare is under control! Only one third of the ventilator machines in Tarrant County are in use, half the hospital beds are filled. We are prepared to care for the sick.
Robert H. Kelly, MD FACP
TOO MUCH INFORMATION
For those with non-insulin-treated diabetes, what is the value of home testing of blood sugar or self-monitoring? Home testing imposes cost and inconvenience on the diabetic. Researchers sought to prove whether self-monitoring finger stick glucose makes a difference.
Robert H. Kelly, MD FACP
PMH QUOTATIONS
"So, this is what it means to be a physician – to uphold long traditions of professional obligation and maintain focus on the needs of each individual patient, and to protect the sacred covenant between patient and the physician."
Thomas L. Schwenk, M.D., 2020
“Three fifths of the practice of medicine depends on commonsense, knowledge of people, and of human relations.”
Harvey Cushing, M.D., 1921
“Between the patient and the guidelines, there needs to be a doctor that is using his/her brain!”
Joseph Alpert, M.D., 2020
“As a physician, you start observing, gathering clues from the moment you enter the door.”
Sharon Inouye, M.D., 2020
“For at first, neither were the physicians able to cure it, through ignorance of what it was, but died fastest themselves, as being the men that most approached the sick.”
Thucydides, physician, 411 B.C.
PMH STORY
A retired physician in California was increasingly worried about his sister in Fort Worth. The sister had never had children, and she was his only sibling. She designated her brother as her healthcare power of attorney. The brother was now in his 90s, and could no longer travel to Texas to be with her.
The brother faced multiple providers in multiple situations giving complex advice about the sister, which he found confusing and unsatisfactory. She had been in the hospital several times and each time encountering another team of doctors, never the same doctor. It was confusing. Primary care was provided by a home visit service, again several doctors, multiple nurse practitioners, and PAs, who rotated visiting the woman at her assisted living facility.
The family asked the PMH doctor to get involved. Over the next several weeks, the PMH doctor visited the sister at her assisted living facility. The doctor quickly realized that she was no longer suitable for assisted living and would need either memory care or skilled nursing facility. Then behaviors at the assisted living facility led to hospital admission. The PMH doctor saw her in the emergency room and followed her during her hospital stay. At discharge, the sister went to a skilled nursing facility where the PMH doctor was again her physician and made rounds at that facility. The PMH doctor saw the patient before, during, and after the second hospital visit reporting back to the family in California. We call this continuity of care.
While making his visits one morning, the PMH doctor sent a brief video to the family in California, showing the sister’s room, the hallway and the view outside her window. The PMH doctor will continue to visit the sister. During an office visit, the brother joined the sister and doctor on Face Time.
There are times like these when there can be too many doctors, too many communications, and too much confusion. It can be simplified when a doctor and a family agree to work together, and when the doctor maintains continuity of care. This continuity of care was important to the family in California, the family in Texas, and also to the patient with dementia. The sister now recognizes her PMH doctor and smiles whenever she sees him, calling him Doctor. Anonymity and multiplicity have been replaced by continuity by a decision made between a competent, loving sibling and a doctor who knows the patient and has followed her through her hospitalizations.
That’s part of the reason we have created PMH: To value continuity of care and to make the continuity of care available for a fee that is modest and affordable. Whether the fee is a good value will be the judgment of the patient and the patient’s family. If it is worth it, they will subscribe. If it’s not worth it, then they will continue with the prior pattern of care. Giving people the opportunity to make this decision and to make this choice is good.
Allan R. Kelly, MD, FACP
STATIN DRUGS CONTINUE TO BE OUR FRIEND IN NEED
Recent publications looked at the benefit of statin drugs in unexpected places. It will always be true that as many as 10% of patients taking statin drugs will perceive muscle aches and discomfort. It is a balancing act: side effects vs. benefits. There is a benefit to statin drugs with regard to atherosclerosis and cardiovascular disease, but there are also other benefits. This is often referred to as “pleomorphic” benefits of statins. One set of researchers looked at statin benefit in patients with dementia later in life and noted that there was an improvement in behavior and outcomes. An experiment from China randomized patients with subdural hematoma, to the statin Lipitor or to a placebo. There was a distinct improvement in those treated with Lipitor compared to those treated with placebo. Surgery was needed in 11% on a statin, 23% on placebo. There was clinical improvement in 46% of those on the statin but only 28% of those on taking a placebo. A third intriguing recent study looked at C. difficile colitis. This is also uncommon but is less likely to occur in a group taking statin drugs compared to those taking placebo.
Robert H. Kelly, MD, FACP
ASPIRIN LETS US DOWN
The incidence of strokes and heart attacks has fallen for decades in the US. This change now affects the value of preventative aspirin. Two randomized, placebo-controlled trials were published in the October 18, 2018 issue of the New England Journal of Medicine, on the effect of aspirin on the health of persons older than 65 years. In one, nearly 10,000 persons without a history of cardiovascular disease were randomized, one group taking 100 mg of aspirin.
Robert H. Kelly, MD. FACP
REPORT – SIRI VS. ALEXA
A study was done looking at the accuracy of Siri and Alexa in interpreting plain language medical questions. There were 54 subjects who recorded their instructions to the voice assistant.
Robert H. Kelly, M.D.
DON’T FALL DOWN!
Approximately 30% of adults over 65 who live in their homes fell in 2014. Patients living in nursing homes or assisted living facilities have a much higher incidence of falls. Risk factors include, for example, age, some medications, frailty, cognitive impairment or dementia, and other chronic illnesses.
Allan R. Kelly, MD, FACP
DEMENTIA
Treatments have failed; prevention works. Over the past 20 years, extensive research on dementia has focused on treatment, but billions of dollars invested in this research have come to naught. On the other hand, prevention strategies are helpful. Certainly, we know that education, removal of tobacco smoke, and prevention of head injury reduces the risk of dementia. We also know that treatment of hypertension in middle age and into the older years will reduce the lifetime risk of cognitive impairment and dementia. We know that statin drugs in selected high-risk patients, such as diabetics and individuals with high blood pressure, can reduce dementia risk.
Allan R. Kelly, MD, FACP
PMH QUOTATIONS
"The hardest conviction to get into the mind of a beginner is that the education upon which he is engaged is not a college course, not a medical course but a life course, for which the work of a few years under teachers is but preparation."
William Osler, 1895
“A recent study found that US physicians spend only 24% of their time communicating with patients, while a staggering 44% of their time is spent facing computer screens…a highly trained US physician has become a data entry clerk, and this has grim implications.”
Muhammad Khan, MD, 2019
“The Mayo brothers were steadfast advocates for their patients. All faithfully collaborated to establish a broad and enduring covenant to serve others; a commitment to an empathic presence in the face of human suffering; and an abiding trust in the moral foundation of medical caregivers. ”
Editors, Mayo Clinic Proceedings, 2019
PMH STORY
A caregiver at the elderly patient’s home was concerned that there had been a change in mental status. The patient was no longer responding verbally. Her eyes stayed closed and seemed even to roll back when the lids were opened. The member's son was out of town, and no family were available.
Because of my proximity, I was able to visit the PMH member’s house. I knew well the years of frailty, chronic illness, and dependence that had preceded this visit. At her bedside, I saw occasional spontaneous, purposeful movement in legs and hands. I then spoke with her. There was a minimal verbal response, but good vital signs. There was no distress, but a rash around the left eye. The rest of the exam was unchanged from prior visits. The rash had blisters. It was a subtle, early eruption of shingles.
She wanted to be repositioned but asked that she be allowed to return to sleep. This was her usual manner.
The close knowledge of the patient, the ability to visit at the her home, the easy call by staff directly to the doctor: because of this a call to 911, ambulance, hours in the emergency room, and overnight admission to the hospital were avoided. The problem was shingles, which can cause a change in a person's energy and capacity when they become weakened. Shingles was the cause of change in this case, and a trip to the hospital would have been no additional benefit to the patient.
There are house call services available. They may or may not respond to this kind of call. There are other doctors that make house calls. Such care, when practicable, is one of the benefits of Premium Medical Home. A conscientious doctor cannot leave an office with a full schedule - this imposes too much inconvenience on other people. But at other times it is practicable and appropriate and is often useful. Even with the doctor's visit or call, the recommendation may still be an emergency room evaluation because of technology, facilities, and nursing care in the emergency room, which is not available in a person's home. But it is good to know that a preexisting knowledge of the person, a firsthand examination, a thoughtful weighing of pros and cons, and not just a generic guideline, have gone into the recommendation to undertake a trip to the emergency room.
Robert H. Kelly, MD FACP
Fans, Heat, Physiology
We have many ways of adapting to both cold and hot temperatures. Common sense is probably the best way to decide what to do. But researchers can also add to our knowledge.
Allan R. Kelly, MD, FACP
E-CIGARETTES AND CARDIOVASCULAR RISK
The dangers of cigarette smoke are clear. It appears that treatment with e-cigarettes is safer than nicotine satisfaction with combustible cigarettes. We want patients to satisfy their nicotine addiction with a safer product. This can be patches, gum, or even an e-cigarette (vaping). But sometimes patients will use the e-cigarette and NOT stop combustible cigarettes. Research now identifies that this is dangerous.
Allan R. Kelly, MD, FACP
STATINS AGAIN
Statins are proven to reduce the risk of heart attack and stroke. Guidelines have suggested that as we get into our 80’s and 90’s, the value of statins decreases and it would be prudent to discontinue these medications when given for primary prevention (the use of medications to reduce the risk of a first stroke or first heart attack).
Allan R. Kelly, MD, FACP
PENICILLIN ALLERGY
How important is a history of penicillin allergy? If there are breathing problems, low blood pressure, or trips to the ER, for example, then the diagnosis should not be doubted. But for many, the history of penicillin allergy is a memory from childhood or advice from a parent. Penicillin and its related medication are such a useful group of treatments that one would not want to foreclose their safe use.
Robert H. Kelly, MD FACP
SCAMS TARGETING THE ELDERLY
Many of us have heard stories of an older person with mild cognitive impairment becoming the victim of scam or fraud. Research at the Rush Alzheimer's Disease Center in Chicago has shed some light on a possible relationship between scam awareness/resistance and an associated reduction in the risk of Alzheimer's disease. Three basic measures were used, that would predict susceptibility to scam.
Robert H. Kelly, MD FACP
PMH QUOTATIONS
“The scientific literature is replete with good intentions gone awry…Clinicians should continue to provide…care based on existing evidence. Intensive interventions beyond these basic measures warrant additional research and must consider potential harms.”
Seppo Rinne, M.D., Peter Lindenauer, M.D., and David Au, M.D., 2019
“So when [my patient] thanked her family, her friends and her doctors “for literally” giving her life, I wanted to thank her– for giving me purpose, a place in the world, the chance to be part of her life.”
Lisa Rosenbaum, M.D., 2019
“Keep a looking glass in your own heart, and the more carefully you scan your own frailties, the more tender you are for those of your fellow creatures.”
Sir William Osler, M.D., published in JAMA, 1969
PMH STORY
The PMH patient had had recent surgery. He fell and re-fractured his leg. Because of his advanced age, the surgery was complex, involving a rod and wire to hold the badly damaged bone so it could heal around this reinforcement. Recovery was difficult; he stayed in the hospital then went to a rehabilitation facility, and was finally discharged home with home health. Progress was good, but seven weeks later, there was pain back in that same leg, as before. The patient was seen the same day in the PMH office. X-rays showed that the bone was intact: there was no collapse. But the pain was severe, and the PMH doctor made adjustments in the pain medications. At this time, a call was placed to the surgeon.
The next day, x-ray reports and laboratory were back. The patient was calling on the phone, but at the same time, the orthopedic surgeon, whose office was many miles away, returned the call from the day before. The PMH doctor asked that the patient’s call be placed on hold as he talked to the surgeon. He told the surgeon that the patient had developed an unexpected worsening of his pain, and he asked if the surgeon would mind talking to the patient in a conference call. The surgeon agreed, and a conference call occurred between the patient, the surgeon, and the internist. The patient was able to explain his symptoms and what had happened. The internist was able to explain the laboratory results and the x-rays. The surgeon was able to talk to the internist and the patient and make a plan of care. This was a good phone call.
This is a PMH story because of our commitment to directness. Directness includes the desire to use modern tools for better communication between doctors, consultants, nurses, patients, and families. We don’t want there to be barriers. We want to improve communication at the time when it is most valuable.
Experiences like this are good for our patients, good for our consulting physicians, and good for families. Directness is better than indirectness.
Allan R. Kelly, MD, FACP
COGNITIVE FUNCTION AND EXERCISE
There is a great interest in cognitive impairment in the elderly. Researchers at Duke University looked at men and women over 55 years of age who had both cognitive impairment and cardiovascular disease risk factors. They randomized 700 patients equally to four groups: The first group exercised three times weekly for 12 weeks; the second group had dietary counseling roughly once weekly for 12 weeks; the third group had a combination of exercise and diet counseling, and the fourth group simply watched a 30-minute health education video once weekly. The researchers measured executive function and cognitive function. Diet counseling focused on the “DASH” diet (most importantly, a low salt diet).
Allan R. Kelly, MD, FACP
PREVENTING FRACTURES
Women over the age of 65 have a 40% risk of experiencing a serious fracture in their lifetime. There are a lot of common sense things that will help prevent fractures, and there are also medications doctors can prescribe.
Allan R. Kelly, MD, FACP
FRUIT CONSUMPTION VERSUS FRUIT JUICE
Fruits have fructose, not sucrose or glucose as the sugar component. A recent publication in BMJ looked at fruit consumption and the risk of diabetes. Data from three large studies were reviewed, the two largest being nurses health studies done 10 and 15 years ago. Approximately, 12000 patients in these large studies developed diabetes in the course of the study. Three or more servings of fruit per week in the diet were not associated with increased risk for developing diabetes, but there were differences between fruits. There was nearly a 25% diabetes risk reduction in individuals whose fruit consumption was primarily blueberries. Grapes, prunes, apples, pears, bananas, and grapefruit also lowered risk. Peaches, plums, apricots, oranges, and strawberries were neutral. Cantaloupe and melon increased the risk slightly.
Robert H. Kelly, MD, FACP
ATRIAL FIBRILLATION
Recent research from Australia showed abstinence from alcohol in moderate drinkers with atrial fibrillation resulted in a significant reduction in AFib recurrence rate, total AFib burden, and symptom severity. Additional benefits of abstinence included a 12-mm drop in systolic blood pressure and 7-pound average weight loss over the six months trial.
Robert H. Kelly, MD, FACP
VITAMIN E BACK IN THE NEWS
30 years ago, Vitamin E was attracting attention for its anti-inflammatory properties. Benefits were uncertain. As a way to reduce heart disease, it was not helpful. But there is still a role for Vitamin E. A study at the VA about five years ago showed that Vitamin E was as effective as testosterone in relieving symptoms in certain veterans.
Robert H. Kelly, MD, FACP
PMH QUOTATIONS
“Every human being of adult years and sound mind has a right to determine what shall be done with his body.”
Supreme Court Justice Benjamin Cardozo, 1914
“Eating alone will not keep a man well; he must also take exercise. For food and exercise work together to produce health.”
Hippocrates, a physician, 400 BC
“In truth, my failure to meet the local EHR requirements ended my academic practice. The administrative requirements for physicians that are buried in the EHR are now staggering, and the additional requirements inherent in changing reimbursement…are virtually impossible to fulfill.”
Donald Girard, MD, 2019
“Without changes in the values, culture, and environment of care, clinicians in hospitals will increasingly find themselves at odds with patients and family members, who, like us, watch many individuals come and go from their hospital room every day. We can find no one who is ultimately responsible for recovery. Even though I am a physician, I felt like I was standing in front of an express train of technology that I could not stop.”
Lenore Buckley, MD, 2019
ASPIRIN IN HEALTHY OLDER ADULTS: DISAPPOINTING
Aspirin helps to save lives and prevent problems in people with established cardiovascular disease. But people who have no cardiovascular disease and have never had a heart attack or stroke are a much larger population. Should they take aspirin as part of a healthy approach to maturity? The United States Preventive Services Task Force has long recommended balancing of risk and benefit in this healthy group. Aspirin reduces the risk of heart attack and stroke (ischemic events) but also increases the risk of serious problems, such as GI bleeding.
Allan R. Kelly, MD, FACP
Robert H. Kelly, MD, FACP
FECAL TRANSPLANTATION CONTINUES TO SURPRISE
We continue to explore the ways in which our body’s ecology, or biome, affects our health. These terms refer to the bacteria and viruses inside or on our body. The microorganisms in question are fecal microorganisms. Drugs or events that change the microorganisms inside the colon can cause illness. Changing the fecal ecology can have positive or negative effects on health.
Allan R. Kelly, MD, FACP
REDUCING FALLS, IMPROVING HEALTH
As we age, falling becomes common. Most falls do not result in serious injury. But advancing age creates fragility in our bones and muscles and skin: falls are more likely to be injurious.
Allan R. Kelly, MD, FACP
NURSE PRACTITIONERS
An emerging model of care is independent nurse practitioners. They have become particularly important in long-term care and hospital care. Nurse practitioners serve as subspecialty clinicians in pulmonary medicine, intensive care, cardiology, and the emergency room, to name a few.
Robert H. Kelly, MD, FACP
SURGICAL RISKS
Surgery may lead to complications. Fortunately, the risk of death from surgical procedures is extremely low – 1 in 10,000 or less depending on the procedure done. Complications following surgery range from 2%, (minor procedures) to nearly 20% (major procedures). Complications may include pneumonia, infections, confusion (delirium), anemia, kidney impairment, and heart failure.
Robert H. Kelly, MD, FACP
SELF-SAMPLING FOR HPV INFECTION
Human papillomavirus (HPV) infection is the cause of cervical cancer. Testing for HPV measures the risk of cervical cancer. Detection of this virus is the best way to screen for this cancer. In the absence of HPV, cervical cancer is highly unlikely and the pap smear is unnecessary. For women known to have high-risk HPV, a traditional pap smear is needed. The question is whether or not home HPV sampling can be used in place of doctor visits.
Robert H. Kelly, MD, FACP
Allan R. Kelly, MD, FACP
PMH QUOTATIONS
“Developing expertise does not negate the need to retain and nurture the humanity that drove us to medicine in the first place.”
Anna Goshua, MD 2019
“For the sake of our profession, get out of the current EHR rut, and enjoy the balance of the rest of your life as a doctor.”
Andrew Alexander, M.D., (2018)
“When my resolve faltered, I reminded myself that my suffering was trivial compared to that of my patients.”
C. Alessandra Colaianni, MD, 2018
PMH AND HOSPICE – A PMH STORY
One PMH principal is continuity of care by direct relationship with patients and their families. This is especially important during a long and complex illness. It is also important at the end of life.
A PMH couple were ill. The wife had dementia and the husband was the caregiver. But the husband developed pancreatic cancer. The wife was moved to a memory care unit so that the husband could meet with doctors to begin treatment. But treatment failed, and there was no hope for further intervention to prolong his life or to cure the cancer. In time he would lose his ability to care for his wife as he dealt with his own terminal illness. Hospice would be a help to him and the family endorsed this. The family asked, “Dr. Kelly, you will take care of our father when he goes on hospice, won't you?”
That Saturday, Dr. Kelly sent a brief text message to a hematology colleague about the patient and asked if he would be able to see the patient early in the coming week. Records were faxed to the hematologist’s office.
Almost all primary care doctors have given up following their patients on hospice. Often they simply don’t have enough experience, never having served as a hospice medical director nor the time. We have talked to many hospice representatives who tell us it is rare to find a doctor who will follow a patient on hospice.
When the husband transitioned to hospice, the PMH doctor made rounds and talked to him at each visit about his much beloved wife, whom the doctor visited regularly at the memory care unit. When the family came to be with their dying father, they could also talk to the PMH doctor about their mother. This helped them care for their mother and father. They knew that the doctor was there for their mother and father. And the dying husband had confidence that his wife would be cared for.
The father died. The mother lives on with Alzheimer’s, still cared for by the same physician who knew her at a better time, who is able to talk to her about her husband whenever her thoughts turn that way. At times, she still recognizes her doctor.
PMH is about continuity, directness, and willingness to follow the patient even on hospice, which is good for the patient, and the family. PMH gives preeminent importance to the feelings and wishes of the patient and the patient’s family.
Allan R. Kelly, MD, FACP
A VACCINE THAT PREVENTS CANCER
Cervical cancer is a common cause of cancer and cancer death in women. The American Cancer Society for decades recommended annual pelvic exams and every three year Pap smears for women. Cervical cancer deaths in the United States were markedly reduced by screening, but cervical cancer remained one of the top 5 causes of female cancer death despite this effort.
Allan R. Kelly, MD, FACP
UNEXPECTED BENEFITS FROM AN ANTIVIRAL DRUG
In 2013, the first anti-hepatitis C virus antibiotics were approved. These antiviral antibiotics are highly effective with success rates of 98% to 100%. Many people with chronic hepatitis-C are cured within weeks of taking antibiotics. A recent report reveals an additional benefit. There is a shortage of organs for transplantation. Many of the people who die and have organs that would be good for others cannot donate because they have hepatitis C infection. These people died before they were treated and since hepatitis C was present, these organs could not ethically be used for transplantation.
Allan R. Kelly, MD, FACP
NARCOTIC TREATMENT OF PAIN CONTROL
A recent study looked at the effectiveness of narcotic medications for the treatment of musculoskeletal complaints. Patients were randomized to two groups: either treatment with narcotics or non-narcotics for 1 year. Outcomes studied were pain and function.
Robert H. Kelly, MD, FACP
INCREASED RISK CAN MEAN BETTER OUTCOMES:A HIDDEN COST OF FREE CARE.
There are a large number of patients waiting for a transplantable kidney. Donors are rigorously screened for infectious and cancer risk in order to reduce risk: IV drug users, men who have sex with men, and people with certain habits are excluded from the donor pool because of the risk of occult viral infection (HIV and Hepatitis C specifically). Donors with these habits are called increased risk donors. These viruses may be transmissible but not detectable by blood tests. Fundamentally, accepting a transplant from an increased risk donor means to take on a burden of risk or uncertainty about getting Hepatitis C or HIV. This risk could be avoided by waiting for a safer donor. The risk is measurable from these increased risk donors: 1/1,000 risk of hepatitis C and 1/10,000 for HIV infection after transplant. Risk is like a cost the patient has to pay with the coin of uncertainty, anxiety, and possible medical treatment, even though no dollars are paid.
Robert H. Kelly, MD, FACP
PMH QUOTATIONS
“He taught by example, the best of all methods, rather than precept. His associates were deeply impressed by his habits of thought and work; his enthusiasm, his painstaking accuracy, his close observation and his never failing interest in studying problems…”
J.M.T. Finney, M.D., 1940, regarding Halsted, the great surgeon.
“We must be careful too not to lose sight of the fact that we are dealing with human beings, whose individual feelings and interests must ever be respected and guarded. It is axiomatic that the doctor shall be well trained scientifically, but in the treatment of disease, the human element is sometimes of even more importance than the scientific.””
J.M.T. Finney, M.D., 1940
“Teach thy tongue to say, ‘I don’t know.”
Maimonides, a physician, born 1135
“Every patient, even the most degraded…should be treated with the same care and regard as though he were the Prince of Wales himself.””
Joseph Lister MD, 1864
“But the essence of medical ethics, the Golden Rule, has been largely overlooked.”
Michael DeBakey, MD, 1968
“Let it be remembered that the true physician takes care of his patient without claiming to control the diseases in all cases.”
James Jackson, MD, (1856)
PMH FEES
Dr. Robert Kelly's new PMH fees will go into effect
on January 1, 2019 as posted on
www.premiummedicalhome.com
You will be billed for the new rate on your annual PMH renewal date
PMH@Home is for information purposes only.
Consult your doctor for more information
TIMELY CARE - A PMH STORY
The patient was an older gentleman who had been declining in health and vigor. A blood count on Friday showed there was significant anemia. The cause of anemia was not clear.
Dr. Kelly called the gentleman and reviewed the findings, offering to either address this problem in the hospital or at the office. As there were no acute symptoms and the patient lived nearby with his wife, he felt safe at home. Dr. Kelly asked him to start oral treatment for the anemia and return to the office on Monday.
That Saturday, Dr. Kelly sent a brief text message to a hematology colleague about the patient and asked if he would be able to see the patient early in the coming week. Records were faxed to the hematologist’s office.
On Monday the patient came to Dr. Kelly’s office and the findings were reviewed with him and his wife. He was feeling weak. The hematologist’s office had already contacted the patient and told him that he could be seen at 2 p.m. that same day. Appropriate studies were completed and the patient was seen. The correct diagnosis was made and treatment was already underway.
We live in a place where we can get care when we need it and in a manner that we prefer. While sitting in the waiting room the next morning, the patient overheard a conversation: “Isn’t it nice to have a doctor that you can see so quickly?” The day before, his wife had exclaimed, “Thank God we don’t live in Canada!”
This is a story about the care all physicians want to give their patients and the kind of care that patients want to get from their doctor – even in Canada. PMH delivers the opportunity, time, training and experience to organize such care, in a manner preferred by PMH subscribers.
Robert H. Kelly, MD, FACP
IT’S THE PATIENT, NOT THE MRI THAT MATTERS
A study was done of 67 individuals who had never had back problems or sciatica. In The Journal of Bone and Joint Surgery study, three neurologists reviewed each MRI. Volunteers were recruited through advertising, mostly younger than 60 years of age.
Robert H. Kelly, MD FACP
FEED A COLD, STARVE A FEVER
An experiment on mice was done at Yale University. Researchers asked: is there benefit to feeding or not feeding animals infected with virus or infected with bacteria? Half of the mice were infected with bacteria, half with virus. Each group was then divided into two groups: one given food via a tube into the animal’s stomach, and the other given no food, only water. Appetite was poor in both groups, especially in the bacteria infected group. In the bacterial group given nutrition none lived: 0% survived. In the fasting group 40% survived. In the viral group given artificial feeding: none died, 100% survival. But in the fasting virus infected group there were deaths.
Robert H. Kelly, MD, FACP
COFFEE, TEA AND OTHER POPULAR BEVERAGES
We have written recently about the safety of tea. Tea and coffee are among popular caffeinated beverages. The coffee shop and the teapot are icons of western society.
Allan R. Kelly, MD, FACP
OVERDOSE DEATHS AND THE OPIATE CRISIS
Because of the rapid increase in the number of Americans dying from opiates and renewed caution about opiate use, doctors are trying to learn how this trouble came about. In a recent Annals of Internal Medicine, researchers from National Institutes of Health analyzed opiate deaths in 2015 and 2016.
Allan R. Kelly, M.D. FACP
PMH QUOTATIONS
“Doctors who want shift work, who see the relationship with their patients as an arms’ length transaction, who value their private time more than their patients’ comfort, will thrive in today’s world of medicine. But those doctors … have settled for less”
Joseph Mambu, M.D., (2017)
“It is my own practice to avoid drugs as much as possible, and I more frequently find it more difficult to persuade people to abstain from using drugs than to induce them to take drugs.... It is a very narrow and unjust view of the practice of medicine to suppose it to consist altogether in the use of powerful drugs or drugs of any kind. Far from it.”
James Jackson, M.D., (1856)
Guest Editors
Hannah Nguyen, MS-2
Texas College of Osteopathic Medicine
Christina Kelly
University of Texas at Austin
PMH STORY
Continuity of care is one component of good care. We try to use our records, but there is much in life that is not written down or indexed. How much paper and how many computer screens can we look through in trying to make a good decision? But there is also human memory, the knowledge that comes from being with someone, working with them, and getting to know them.
The PMH doctor admitted the patient to the intensive care unit. She had fallen down the stairs, and we suspected that she had struck her head and suffered brain injury. She was unconscious, on life support, unable to breathe or protect her airway, and comatose.
The next morning there was no improvement. Multiple calls were made to the doctor by the Ethics Committee and other members of the team at the hospital. The suggestion was to stop life support. As it happened, Dr. Gordon Kelly was retired but in the office having a cup of coffee. He had known this patient for decades. The PMH doctor asked Dr. Kelly if he would like to make rounds. He said yes.
We went up to the intensive care unit. There was a crowd outside the door and inside the room: the pulmonary specialist, the neurologist, the nursing team, and family. The nurses and neurologist went through a detailed presentation of what had been happening since the patient was found on the stairs. The prognosis was grim. The assembled professionals thought that the ventilator should be stopped and care withdrawn. At this point, Dr. Gordon Kelly made the following comment: This is exactly what happened to her after her aneurysm surgery in 1990 resulted in a series of seizures.
We had no paper or computer records from 1990. The family could not remember what had happened in 1990. With Dr. Kelly’s recollection of those events, we concluded that a possible diagnosis was seizure with postictal coma. We decided to continue supporting the patient. Over the next three days, the woman regained consciousness, was able to be taken off the ventilator, and she lived happily with her family at home for another 7 years, up on her feet and back to life.
This is a story of continuity that changed the minds of everyone in the room, and it changed the life of a family. Continuity in smaller doses and less dramatic fashion is helpful to nurses, doctors, patients, and families.
Allan R. Kelly, MD, FACP
TEA CAN ALSO BE A FRIEND
Tea is the most widely consumed beverage worldwide. Where more tea is consumed, there is less heart disease, perhaps because tea replaces soft drinks or alcohol, but it may be because there is something good about the tea itself.
Robert H. Kelly, MD FACP
NARCOTICS FOR PAIN
New research continues exploring narcotic therapy for pain. Narcotics as opium have been available to humans for thousands of years. Opium consists of equal amounts of codeine and morphine. It is easily available throughout the world.
Allan R. Kelly, MD, FACP
Robert H. Kelly, MD, FACP
TOO MUCH INFORMATION
For patients with non-insulin-treated diabetes, there may be no benefit to home testing of blood sugar. The dogma is that diabetics should do self-monitoring, “an important complement” to measurement of A1C. But finger stick glucose monitoring imposes cost and inconvenience on the diabetic. Researchers sought to prove that self-monitoring makes a difference.
Robert H. Kelly, MD FACP
SHINGLES VACCINATION
There is a new shingles vaccine that the Centers for Disease Control recommends for everyone over 50.
Allan R. Kelly, MD, FACP
CHRONIC BACK PAIN
In Portugal, 97 patients with low back pain were randomized. Half got a placebo and were told the pill was a placebo. Half got no pill at all.
Robert H. Kelly, MD FACP
PMH QUOTATIONS
“The landscape in which medicine is practiced today presents a moral hazard for most practitioners. The rules are set in the boardrooms, the paycheck guaranteed and the creative tension at the bedside vanquished. The result is a joyless practice of medicine devoid of medicines’ artistry and burgeoning with frustrated physicians…”
Joseph Mambu, M.D., 2017
“The sick room is the field of your labors. To everything which occurs there you are to give your attention and every step there should be under your direction. Questions of the deepest importance are constantly arising there for your solution….Let it be remembered that the true physician takes care of his patient without claiming to control the diseases in all cases….The true physician on the other hand cannot fail to be modest in his pretentions; for he is aware how his knowledge and power are limited while he feels the magnitude of his task.”
James Jackson, M.D., 1956
PMH STORY
Premium Medical Home doctors remain active in the medical community.
Recently, I was asked to care for a hospice patient (whom I had never met) admitted to a nursing home. The resident was totally dependent upon her daughter and was in for a short respite stay. After visiting the patient and the nurses, I called the daughter.
On identifying myself to the daughter, the daughter was confused. She said, "Had there been an emergency?" I advised that there had not. She said that in the years she had been providing the care for her mother, including in and out of hospitals and nursing homes, a physician had never called her on the phone.
This is not the first, nor will it be the last, time that a family member expresses surprise and, naturally, appreciation for a doctor's personal attention to their loved one. I shared with the daughter my own personal experience serving as my father's physician. In his last months while in hospice, he had a problem and I was unsure how to proceed.
I called one of the specialists here in town and left a message on their answering service: I was just another patient's family member asking for help. Within minutes, the doctor called me back. We reviewed the issue and he stated that it sounded like I was doing the right thing. He offered to come over or see my father, or have us visit the next morning in his clinic. With the phone call, I had the information I needed and a visit was not necessary. But like the daughter of this hospice respite patient at the nursing home, like any of us when we are sick and do not know for sure what is wrong and what to do, I felt deep appreciation for this doctor who was able, willing and available to help, and willing to talk to me on the phone. We have experienced both sides of the relationship. We want our patients and families to have that support and relationship always at hand.
Robert H. Kelly, MD, FACP
WHAT IS BEST FOR PAIN?
People have been using narcotic analgesics for thousands of years. But are the narcotics any better than new drugs, such as ibuprofen and acetaminophen?
NEW BLOOD PRESSURE GUIDELINES
The American College of Cardiology and the American Heart Association issued new guidelines for the diagnosis and treatment of hypertension. For most of our patients, there will be little change. There are two groups that will notice a significant change.
DO ANTIDEPRESSANTS REDUCE DEPRESSION IN PATIENTS WITH COMPLEX CHRONIC ILLNESS?
Major depression is frequently experienced as a lack of interest in anything that would generally bring pleasure and as an unexplained sense of persistent blueness and depression. Treatment of depression is important. But randomized controlled trials of depression exclude patients with chronic and serious illnesses: cancer, heart disease, kidney disease, and others. Facing such serious illness, patients and their families commonly ask about treatment of depression symptoms.
COFFEE – STILL OUR FRIEND
In a randomized controlled trial, heart patients in Brazil were off coffee for 7 days. Then each person took five doses in 5 hours of 100 mg of caffeine as coffee. This is about the same as five 8-ounce cups of coffee. The placebo group drank coffee. Blood tests, electrocardiogram and stress tests were done. The results showed no adverse or positive effect of coffee on skipped beats, duration of exercise, heart rate, or blood pressure. People like coffee, and it appears that coffee is not dangerous, even in the face of heart failure and arrhythmia.
OSTEOPOROSIS
Long term prednisone use causes a 60% - 100% increase in fracture risk. An experiment was done with 3600 patients in Sweden who were taking prednisone. Fosamax or placebo was started 1-3 months after the initiation of prednisone. Over the 1.3 years, there was a hip fracture rate of 9/1000 in the Fosamax group versus 27/1000 in the placebo group.
PMH QUOTES
"I have come to believe that patient trust in the physician is one of the most important therapeutic elements in our armamentarium. Such trust can be built only when a lasting relationship is forged between the patient and the physician."
William Mayo, M.D.
"Many chronically ill elderly patients should be spared from spending their last hours in the grip of medical technology."
Michael Gordon, M.D., 1985.
"There is building resentment against the shackles of the present EHR; every additional click inflicts a nick on physicians’ morale."
Donna Zulman, M.D., 2016.
PMH STORY
HOSPICE
By now, all older adults know that hospice is a choice they may consider for themselves or their loved ones as illness progresses and goals change.
The PMH patient was an elderly gentleman with progressive neurological disease causing paralysis. His wife had worked for years to care for him at home even as he became bedfast. The spouse took beautiful and effective care of her husband.
As he worsened, he could no longer breathe adequately. Should he transfer to the hospital for usual, aggressive care, or remain at home? The PMH doctor met with the family and the patient in the emergency room. Respiratory failure was impending. At the ER, we could quickly assess that this was nota reversible disease. The patient and his wife were asked, "Do you want to be cared for at home or do you want to be cared for in the hospital?" Both firmly expressed they wanted him to be cared for at home. A daughter, in the room, also wanted his care at the home. With this decision, hospice was offered and a referral completed.
His PMH doctor talked to the hospice team before he left, and also talked to the familyabout his condition and family goals and wishes. The family returned home but delayed starting hospice; "it didn’t feel quite right." She wanted to think about it another day or two.
Two days later, she called and said she wanted to talk to a different hospice company and the PMH doctor made that referral. The following day, the hospice referral was completed and the family had signed up with the hospice company. Thankfully, the family had the time at home that they treasured.
The patient's wife and children needed time, conversation, and the options to explore their own best choice and their own feelings and decisions. The time required to explore and understand is important and worth taking.
We believe that where there is good communication between patient, doctor and family, the decisions will be more gentle, more careful, and better for all concerned. This is why we have created PMH. We want the patients and families to have time, attention, and thought appropriate for the difficulty and magnitude of the decisions they face.
Allan R. Kelly, MD, FACP
PMH FEES
A REMINDER - Dr. Allan Kelly's new PMH fees went into effect on October 1, 2017. They are posted on our web site, PremiumMedicalHome.com and are also available by calling the office. You will be billed for the new rate on your annual PMH renewal date.
Allan R. Kelly, MD, FACP
EXERCISE, COGNITION AND FALLS IN OLDER ADULTS
Falling is a big problem for the elderly. Falling can cause injury and loss of independence,and force a move out of the home and into assisted living.
Allan R. Kelly, MD, FACP
REDUCING NURSING HOME HOSPITALIZATIONS
Medicare wants to reduce the hospital admissions of nursing home residents. Currently, admissions are based on judgment by nurses and physicians depending on patient needs.
Allan R. Kelly, MD, FACP
CORTICOSTEROIDS FOR IRRITATING COUGH
Patients with asthma predictably respond well to steroid therapy along with antibiotic treatment for acute bronchitis. About 15% of adults without asthma who have a lower respiratory tract infection (like bronchitis or a cold) are treated with corticosteroids. But after the acute infection, some are often left with lingering cough. The role for antibiotic treatment is negligible in reducing symptoms. Would steroids help reduce these symptoms in the person without asthma?
Robert H. Kelly, MD, FACP
OSTEOARTHRITIS
The National Institute of Health and Duke University studied whether intensive and complex intervention for the treatment of osteoarthritis, (a universal, degenerative condition)can make a difference
Robert H. Kelly, MD, FACP
PMH QUOTATIONS FALL 2017
"The experience in that tiny hut [in Africa] was a reminder to stop talking, be still, and focus on the patient. The patients will tell us what's wrong with them if we listen." Ann Elise Kutzler, second year medical student, 2017.
"Listening and thinking are still what patients expect from their physicians."
Frank Sparandero, M.D., September 2017
"No disease that can be treated with diet should be treated by any other means."
Maimonides. A Physician, 1135-1204 AD
PMH STORY
Premium Medical Home is a way of running our offices and serving the public that we think is better. PMH principles are professionalism, directness, continuity of care, and enough time to give care. The fifth is affordability.
The PMH member had retired. He was careful with his money, as we all try to be, so he was surprised when he went to pick up a refill of his medications. He found that a medicine that had previously been affordable was now expensive, $300 for three months instead of $50. He called pharmacies that used his insurance and found a similar price. Knowing that his PMH doctor is committed to affordability, he called the doctor's office to ask for advice.
The staff and the doctor are aware of the financial problems and cost problems that patients face. Getting a call like this from a member is not unusual. He lived in another city, so the office called the lower cost retailers in that city and asked for a cash price. What would it cost to just buy the medication if you had no insurance at all? We found that Costco offered the product for a cash price of $30 for three months. We called the member, we sent the prescription to Costco, and the member's medical care became more affordable.
Affordability is a complex topic. At PMH we focus on affordability, like accepting insurance. We also try to be aware of what cost choices there are out there, and to pay attention to the relative benefits and risks of the drugs we prescribe. We don’t know when our members will face affordability issues, but we will help them when this arises.
Allan R. Kelly, MD, FACP
NEW ANTICOAGULANTS: XARELTO, ELIQUIS, PRADAXA vs. WARFARIN
We continue to see information on new drugs for anticoagulation. Atrial fibrillation can cause blood clots and strokes.New anticoagulants have been licensed to reduce this stroke risk. Researchers in the Journal of the AmericanCollege of Cardiology, 2016 reviewed the impact of new oral anticoagulants on all-cause mortality compared with warfarin. Looking at over 70,000 individuals who were taking one of the anticoagulants, the all-cause mortality rate during the course of the study was 8% in the new anticoagulants, and 9% in the warfarin group.
OBESITY SURGERY AND DIABETES
We continue to watch the development of treatment for the extremely obese persons with body mass indexes over 40. The Mayo Clinic has recommended gastric bypass surgery for decades for patients whose obesity problems have become unsupportable.
STEM CELLS
There is much interest in stem cell injections for degenerative joint disease. Attempts have been made to use stem cells to treat other age-related diseases. In the New England Journalof Medicine, a study looked at two patients cared for at a university in Japan. Vast efforts were made by a large team of specialists ethically using stem cells to reverse macular degeneration – the efforts failed. Other stem cell research in the eye has failed dramatically.
TESTOSTERONE AND MALE AGING
In a recent experiment, 170 men were randomized to testosterone or placebo to see the effects of testosterone replacement on coronary artery calcification or plaque. Testosterone effects on cholesterol plaque were measured by CT.
SKIPPING BREAKFAST
There has been talk about the benefit of eating breakfast when weight loss is desired: You have to eat breakfast if you want to lose weight, some said. This has been called into question with recent research.
KNEE ARTHRITIS
For decades, doctors have used intraarticular joint injections to try to relieve pain in people with chronic arthritis. However, the development of new imaging techniques and our ongoing commitment to experimental methods have led to new insights in the use of steroids for knee arthritis.
PMH QUOTATIONS
"I now see that the medical system is layered to shield the doctor from direct contact with the patient (except for the appointment time)."
Carl Norden, M.D.,2016
"I’ve learned to be intolerant of stereotypes, to recognize that every person has a unique story. When we are privileged as physicians to hear another person's story, we shouldn’t take it for granted."
Adam Hill, M.D., 2017
"This total commitment to the welfare of the patient has been undervalued in the formulation of ethical guidelines, whereas the assumption that such personalized care would be provided by the healthcare system has been over credited."
Chris Feudtner, M.D., 2001
PMH STORY - THANK YOU
A big and heartfelt thank you to all of our patients and their families.
For many years, we have invited medical students to work in our offices. We want medical students to have the opportunity to work with internists who are active in their community, office, nursing home, hospital, and other facilities where our patients receive care. This is a voluntary effort on the part of the doctors. No reimbursement or payment is sought or expected, and the experience contributes to education and training of doctors for the future. Our work is endorsed by UNT Health Science Center (we are both adjunct clinical assistant professors) and by The American College of Physicians where Dr. Allan Kelly received the Texas Chapter Emerald Award for service in education.
It is your choice whether to allow the student to be part of your care. We believe that having a student involved does not distract from good care and at times has positively contributed. There will be times when a patient doesn’t want a student involved, when they don’t want to meet a new person, when they just want to work with the doctor with whom they are familiar. When a student is introduced to participate in your care, please don’t hesitate to say you would rather see the nurse or doctor. At times when you are open to working with these young people, we thank you very much. We aim to limit student participation to just two or three months out of the year.
Premium Medical Home is about running an office in a way that is good for our patients, their families, and the community. Helping young doctors and encouraging them to work in our city is good for everyone.
Allan R. Kelly, MD FACP and Robert H. Kelly, MD FACP
FALLS
When you are young, falls are embarrassing, and sometimes may be dangerous. At any age, no one wants to fall and all of us want to avoid injury.
As we age, falls are more likely to be dangerous and should be reported to your doctor. Your doctor will then likely consider what may have played a role in the fall and what measures can be taken to avoid future falls. At any age, medications should be reviewed. Strength and balance training may help.
READY FOR DISCHARGE?
When a person is admitted to the hospital, there may be uncertainty whether they are ready to go home when discharge arrives. The doctor and the nurses may all feel good about that discharge, but from time to time the patient or the family is not so sure and wonders if they are being sent home too soon. A recent report in The American Journal of Medicine looked at all discharges from hospitals in Edmonton, Alberta from October 2013 until November 2014. Patients discharged were questioned about whether or not they were ready for discharge. Twenty-three percent of patients discharged reported "being unready for discharge." Being unready for discharge was associated with disability, cognitive impairment, dementia, poor education, and multiple hospital admissions. But the risk for hospital readmission and the risk for death did not differ between the two groups over the course of the next 30 days. Specifically, only 15% of those who felt unready for discharge were readmitted, versus 18% of those who felt ready for discharge.
OVARIAN CANCER SCREENING DOES NOT WORK
Doctors recommend cancer screening in order to reduce death rates and disability from cancer. We have found that cancer screening is successful for some cancers, but not for others. One of the most important lessons of the past 20 years is the failure of ovarian cancer screening. An American study published in 2011 randomized 68,000 women between ages 55 and 74 to screen for ovarian cancer with combined blood testing and pelvic sonography. There was no difference in death rates, nor was there any difference in stage of cancer upon diagnosis. The screening failed to save lives.
METFORMIN AND COLON POLYP PREVENTION
It looks like a common medication, metformin, may reduce colon cancer risk with medical treatment. In a recent experiment, people who had had polyps removed at colonoscopy were told to come back in one year. One-half of these persons were randomly assigned to take metformin 750mg daily; the other one-half were given placebo.
NARCOTICS AND CHRONIC PAIN
In persons suffering chronic back pain, hydrocodone (an opioid narcotic) was compared with placebo to see if it was effective for chronic pain control. Pain was measured on a 100-point scale: a change in pain score of 20 points was considered significant. Nearly 50% of patients treated with hydrocodone, compared to placebo, withdrew because of side effects. Moreover, those continuing to use hydrocodone did not receive significant pain relief. Opioids, compared to placebo, reduced pain insignificantly for those patients with back pain. Other research shows that long acting opiates appear to increase the relative risk of death more than 50% compared to persons whose back pain is treated with antidepressants or medications such as gabapentin.
PMH QUOTATIONS WINTER 2017
"Clinical excellence remains the best medicine."
Burke Cunha, M.D., 2017
"I now see that the medical system is layered to shield the doctor from direct contact with the patient (except for the appointment time)."
Carl Norden, M.D., 2016
"The computer has taken over our offices. This rise of the machines…has led to more and more angst and physician burnout…we work harder, with longer hours, and more time doing meaningless, useless tasks. The physician patient relationship has been eroded almost irreparably because we so often spend too much time staring at computer screens and not enough time actually connecting with those we serve."
Hujefa Vora, M.D., 2017
PMH STORY
PMH is about continuity and knowledge.
The patient was in his early 90's. The PMH doctor cared for the man and his wife for over 20 years. The wife died 15 years ago. Family always thought the PMH doctor took good care of mom, even though she died, and always had confidence in the doctor's care of their father.
A gradual downhill course eventually pointed to approaching end of life for the father. His illnesses were severe. He was comfortable and surrounded by his family in the hospital room. But it was time to confront that there was nothing else that the doctors could do to get him back on his feet and to recover his strength.
In a meeting with the family, the doctor was able to recall the patient's history dating back decades, to reflect upon the spouse's death, and to talk about the future and how to take good care of a good man, even at the end of life. The doctor had cared for the patient in the office, at the nursing home, and was sitting at the patient's bedside in the hospital. With transition to hospice, the doctor would again be by his patient's side.
The trusted and longtime physician at the patient's bedside is valuable, a good thing. Regardless of what may be happening elsewhere in hospitals and nursing homes, at PMH we are committed to this continuity of care over time. We believe continuity of care is good for the patient, the family, the doctor, and those who support the patient, even at the end of life.
Allan R. Kelly, MD FACP
ANNOUNCEMENT
Dr. Robert Kelly's Subscription Fees will be increasing as of January 1, 2017. The new fees are posted on our web site, www.PremiumMedicalHome.com and are also available by calling the office. As your PMH renewal becomes effective, you will be billed for the new 2017 fees.
BLOOD TRANSFUSIONS: IS BLOOD FROM MEN AND WOMEN DIFFERENT?
In the popular media there is all this talk about gender, malehood, femalehood, etc. Doctors have always known the truth: There is a difference.
But even we were surprised when JAMA 2016 presented data on male and female blood donors. The advent of big data has allowed for tracking outcomes in new and comprehensive ways.
ANTIBIOTIC TREATMENT: SHORTER CAN BE BETTER
We all remember the doctor's instruction when we had strep throat infections: Take the antibiotics for ten days until they were all gone. Children and young parents became accustomed to the idea of taking antibiotics for one to two weeks, even after we got better.
But times have changed. Over the past fifteen years, multiple studies have compared shorter versus longer courses of antibiotics. Dr. Brad Spellberg recently reported experiments of shorter versus longer duration therapy. For example, in community-acquired pneumonia, stopping antibiotics after five days was superior to continuing antibiotics for 7 to 10 days. Other studies included pyelonephritis (7 versus 14 days), intraabdominal infection (4 versus 10 days), sinusitis (5 versus 10 days), and cellulitis (6 versus 10 days). According to Dr. Spellberg, shorter duration beats longer duration in these clinical syndromes. I believe these new studies will lead to a change in clinical practice.
PAREGORIC, OPIUM, MORPHINE: PAST AND PRESENT
Paregoric represented an ancient tradition of care, its components in use for thousands of years. The active ingredient is a natural product from poppies, and used by people of all social statuses, all incomes, and all educations in every country since the time of Marco Polo.
Older people may remember paregoric, used for many purposes in the home. It was used for a teething child who was restless or uncomfortable with colic. It was used for people with diarrhea and stomach cramps and pain. It was available without a doctor's prescription at every drugstore. Mr. Bill Whitten, a pharmacist who built up Whitten's Pharmacy chain in Fort Worth, said he always had paregoric available over the counter. He would keep an eye on it, and if he thought that a person was buying too much, he would turn them away.
INFECTION – WARNING SIGNS
Paying attention to a worsening infection before it requires hospital care is important. One key to transition between infection that can be treated at home and infection that requires hospital care is when infection changes to a syndrome called sepsis. Sepsis is a serious problem with a mortality rate of 15-30%.
REDUCING COLON CANCER RISK
Prudently reducing the risk of colon cancer and colon polyps is important. Cancer tends to develop in a polyp, so reducing polyp formation is desirable. Though the frequency of colon cancer is relatively low for any individual, colon cancer ranks third after breast and lung cancer as a cause of death from cancer in the United States.
Americans are open to medical treatment that reduces risk. Examples are low-dose aspirin and statin drugs for those at risk for coronary disease, tobacco cessation, and bisphosphonates for osteoporosis. And now, maybe metformin for colon polyps. A recent experiment in Japan recruited persons with high risk of forming colon polyps and randomly assigned them to two groups. One group was given metformin 250 mg daily (lower than used for diabetes) and the other given placebo. Colonoscopies were performed after one year. The number and prevalence of adenomas and polyps was then measured and found to be significantly lower in the metformin group. In the metformin group, only 38% of persons had some form of polyp or adenoma on the follow-up colonoscopy, whereas nearly 60% in the placebo group. The risk of colon polyp or adenoma was reduced by almost half.
PMH QUOTATIONS FALL 2016
"The true core of good medicine is not an institution but a relationship, a relationship between two human beings. The better those two human beings know one another, the greater the potential that their relationship will prove effective and fulfilling for both."
Richard Gunderman, M.D., 2016
"He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all."
William Osler, M.D., Aequanimitas, 1904
PMH STORY
The patient was in her 90's. She had been the caregiver for her husband. He passed away, and she had lived now a decade as a widow.
The patient had been part of the PMH practice since 1985, and before coming under the care of the PMH doctor, had been under the care of that doctor's father.
The patient's dementia had been inexorable, causing gradual loss of ability to care for herself, to recognize people, and to understand what they were doing. She moved from her home to assisted living, then to a nursing home, and then to hospice. She could no longer walk. She had neither children nor brothers or sisters in the area.
The doctor had cared for her at the office, the hospital, the emergency room, at the home, the assisted living facility, the nursing home, and now in hospice. Despite all these changes, her doctor did not change.
After she moved to hospice, the PMH doctor came to see her. She was in a wheelchair in a common area. He asked her how she felt and she did not answer. She seemed not to focus. He said to her, "Do you know my name?" She looked up, smiled and said, "Allan Rowan Kelly."
What does it mean to a patient with severe dementia to know the doctor who comes to her side? How important is it? In some practices, doctors do not have the opportunity to ponder this question, as they do not maintain that continuity of care from place to place and time to time. But for the PMH doctor, he felt that it was a balm for this person to recognize him, to see his familiar face, to speak a familiar name, and to smile.
As doctors, we are grateful to be able to care for those who know us and have trusted us for years. It gives meaning to our work. If we must care for strangers, so be it: It is good to care for the stranger. But it is also good to care for those we have known over time. It is important to our patients, and it is important to our doctors and nurses. We call it continuity of care, but it is a basic principle of PMH. Continuity of care is important, valuable, and helpful.
Allan R. Kelly, MD FACP
PALLIATIVE CARE By Allan R. Kelly, MD FACP
Over the past 15 years, a loss of continuity of care and other changes in medical care have led to the creation of palliative care teams in hospitals. Do they help?
The National Institutes of Health funded a large and expensive study at multiple sites in the United States, including Harvard, National Institutes of Health, and Cornell, to see if this concept worked (Carson, et al, JAMA, 2016). The study randomized 365 families whose loved ones had been in the intensive care unit for at least 7 days. Half of the group received usual care from the doctors and nurses in the ICU. The other half received usual care plus palliative care intervention, a complex effort including "…brochures…coordinators…information team…palliative care physician…nurse practitioner…social workers…chaplains…or other disciplines." This palliative care team met with the family of the sick patient in the ICU: "These important information meetings were structured according to a set of objectives and recommended topics…they were allowed some flexibility for adapting the content of the meetings to the particular needs of each family." Everyone involved had a major stake in the outcome. Massive amounts of money were spent.
BASIC LIFESUPPORT? ADVANCEDLIFE SUPPORT? IS LESSMORE? By Robert H. Kelly, MD FACP
It is often worth questioning assumptions. One assumption is that advanced life support (ALS) provided by ambulance personnel will be superior to basic life support (BLS). This question was addressed in a recent study of emergency medical care given to Medicare beneficiaries by emergency medical personnel (EMS). Sixty-five percent of the EMS crews were ALS trained. Thirty-five percent were BLS trained. Was ALS or BLS better? Did higher level training (ALS) of ambulance crews improve outcome?
ZIKA VIRUS IN TEXAS – WHAT IS THE RISK? By Jacob Underwood, MS2 and Robert H. Kelly, MD FACP
Zika virus is spread to humans through the bite of an Aedesegypti mosquito which became infected itself by biting a human with the virus in their blood – whether that human was having symptoms or not. The virus can also spread from person to person through intimate contact. In July, Utah reported a case without known mechanism of transmission. In August, Miami reported mosquito transmission in the U.S.
NOT TOO BUSY By Allan R. Kelly, MD FACP
The patient was a female physician in her late 70's. She had a perplexing syndrome of chest pain. After a stay in the hospital, there was still no specific diagnosis. She made a new patient appointment with a PMH doctor.
The PMH physician was part of the medical staff at the same hospital and so directly accessed her medical records.
PMH QUOTATIONS Summer 2016
"A good physician treats the disease; the great physician treats the patient who has the disease."
Bennett Clark, MD, 2016
"And since we’ve come to think of the hospital as serving the function of a train station – moving people down the line as fast as possible – we shouldn’t be surprised to learn that some patients’ experiences in the hospital have all the warmth of rush hour in Penn Station."
AmandaFantry, MD, 2016
"Sure typing is a little bit faster, but I’ll bet a lot of doctors agree that their clinical thinking was better when their notes were scrawled long hand"
B. Ryan Brady, April, 2016
PMH STORY
A woman in her late 70's was having trouble breathing. Her cardiologist referred her directly to a pulmonary specialist who prescribed three different inhalers and multiple tests. The patient tried taking the prescribed medications. She felt certain that the medications were of no help, and made her feel worse instead of better. She did not call the pulmonologist's office or staff or report the problems with her new medications. Neither did the husband or the patient receive reports or a call with results of the diagnostic studies that were done. Three weeks later, driving to the pulmonologist's office for a follow-up appointment, the patient became more short of breath and decided to go directly to the emergency room. In the emergency room, it was clear that her problems had grown much worse, and her PMH doctor was called.
The PMH doctor saw the patient in the emergency room and cared for her in the ICU over the next several days. The husband complained to the doctor about their experience with the pulmonary office.
It is not easy to complain. If you know you can tell your story to someone and not be seen as a complainer, you can tell your story in more detail and with confidence. Hearing the complaints of the patient's husband was very helpful to the PMH doctor, and was helpful to the pulmonologist and the pulmonology team to understand how they might better serve other patients.
The nature of the PMH practice allowed the patient and her husband to feel entitled to express themselves fully to their doctor. They know their doctor. Working with a doctor over time, knowing that the doctor will join you when you are sick in the hospital or the emergency room, and knowing that you can express yourself fully without judgment, can help everyone.
Allan R. Kelly, MD, FACP
THE MEDITERRANEAN DIET By Allan R. Kelly, MD, FACP
Almost a decade ago, Spanish doctors started the PREDIMED Study on the Mediterranean Diet versus a low fat diet to answer the question, "Can diet recommendations change health outcomes?" Investigators in Spain looked at 7147 persons between the ages of 55 and 80 years. Group one received a low fat diet teaching. Group two received a Mediterranean Diet teaching plus 5 ounces of free mixed nuts per week. Group three received the Mediterranean Diet instruction plus 1 liter of extra virgin olive oil (EVO) per week to be used by themselves, family, and friends.
DAYLIGHT SAVING SYNDROME By Robert H. Kelly, MD, FACP
There may well be differences of opinion, but transition to daylight saving time may not be a harmless government regulation. Not only does it require every American to take time out to reprogram clocks and watches (fortunately, our computers and iPhones can do this on their own), but it appears to have adverse health effects. A recent study (Cipila, et al) was presented at the 2016 American Academy of Neurology Annual Meeting in Vancouver, Canada.
BREAST CANCER SCREENING By Allan R. Kelly, MD, FACP
All women know that for years prudent self-care included breast cancer screening. Since the 1980's, women have been told over and over again to learn about breast self-examination, to have an annual physician examination of the breasts, and to have an annual mammogram in order to follow the guidelines of the American Cancer Society.
PMH QUOTATIONS Spring 2016
"A good physician treats the disease; the great physician treats the patient who has the disease."
William Osler, M.D.
"Almost all the current practicing physicians at Dallas Diagnostic Association have reported decreased productivity and decreased satisfaction with the practice of medicine due to burdens imposed by EHR. Dallas Diagnostic Association experienced the premature retirement of 12 physicians in large part due to the adverse impact of EHR."
Lannie Hughes, 2016 (BUP 29, 2)
"Rather than sitting at the bedside and sharing the suffering of the patient, physicians now spend their time in clinical foxholes on computers and cell phones focusing more on the disease than the person or on technology than touch. . . Just remember the doctors of old – Model them and you’ll be fine."
Paul Rousseau, M.D., 2016 (JAGS, 64, 645-6)
PMH STORY
The PMH Story section has been a place where we have written about how our model of medical care benefits subscribers. We certainly try to look at things from the patient's, not the doctor's, point of view, although the two are closely aligned. We would like to invite any subscriber to submit a brief description of what PMH means to them. What does PMH do for you that is meaningful and desirable and is not generally available in a non-PMH practice?
You may submit these anonymously. Understand that if we do have a chance to publish this, we will change names and dates (and sometimes even gender) to make sure that the patient cannot be identified as a unique individual in our practice though the story will be true and unique.
DEHYDRATION AND HYPERTENSION MEDICATIONS
Every summer we see patients who have fallen or fainted due to dehydration. Here's a heads up to stay healthier during hot weather. A recent correlation has been made between summertime and increased risk for dehydration and fainting-syncope. Fainting spells accounted for 700,000 emergency admissions last year in the USA. Problems with dehydration accounted for at least one-quarter of these. In Arizona, it is called "summer syncope syndrome." Key features include low blood pressure and blood pressure that falls when standing up. The most common symptom is light headedness.
BACON GETS NO RESPECT BY Robert H. Kelly, MD FACP
The World Health Organization recently called red meat a probable carcinogen and processed meat as a known carcinogen. Other known carcinogens include asbestos and tobacco. If a drug was a known carcinogen, the FDA would likely not approve it for sale. And yet, of course, many of us enjoy red meat and processed meat. One wonders if there is a certain degree of anxiety at the World Health Organization.
TRANSPLANTATION: BLOOD, PLASMA, STOOL By Allan R. Kelly, MD FACP
The development of transfusion and transplantation is one of the great triumphs of modern medicine. All the way from plasma for hemophiliacs, to skin for burn victims, or a whole heart, the ability to donate a healthy organ to another in need is a good thing. Doctors are now studying stool (also called fecal) transplants.
HERNIA REPAIR…WITH MOSQUITO NET By Allan R. Kelly, MD FACP
Why is American medical care more expensive than in other countries?The January 14, 2016 New England Journal of Medicine may shed some light. Lofgren and others performed a "randomized trial of low cost mesh in groin hernia repair." The authors compared two types of mesh for hernia repair. One type of mesh was produced by a prominent medical products company, Covidien. The second mesh used in this randomized and controlled experiment was a simple mosquito net produced by a plastics company in India. The Covidien mesh was polypropylene. The Indian mesh was polyethylene. The Covidien mesh cost $125.00 when purchased in Uganda. The Indian mesh was less than $1.00 for an entire mosquito net. The mosquito net was cut up into smaller pieces which were washed and sterilized.
OUT-OF-HOSPITAL OR IN-HOSPITAL BIRTHS By Allan R. Kelly, MD FACP
In our modern world there is a paradoxical interest in out-of-hospital births for pregnant women. Pregnancy and delivery are not common issues at PMH, but I thought our readers would be interested because,for some patients, out-of-hospital birth is considered highly desirable.
PMH QUOTATIONS Winter 2016
"The death of common sense is neither pretty nor fast…we are distracted by the need to fill out irrelevant information and are subsequently left with less time to get through the important parts of our visit."
N. Skolnik, M.D. and C. Notte, M.D., 2015
"As with most guidelines, these [COPD exacerbation preventing guidelines] can be a bit monotonous and hard to read if your goal is to stay awake."
Douglas Paauw, M.D., 2015
"I have witnessed the peace, the comfort, the joy, and the sense of completion when a person chooses to live unencumbered by the demands of modern medical therapy."
Larry D. Cripe, M.D., (2016/01) JAMA, 315 (3), 266.
PMH STORY by Kristina Barsten, MS-IV TCOM Class of 2016,UNT Health Science Center
As a fourth year medical student at the UNT Health Science Center in Fort Worth, I have had the opportunity to rotate through several of the hospitals and clinics in the DFW area over the past year and a half. Spending the month of August in Dr. Robert Kelly's practice, however, was the first time I experienced the model of medical care like that provided by Premium Medical Home.
The comprehensive and coordinated care provided with this model impressed me and was different from mainstream medical clinics I had seen. It allows for the primary physician, the individual most familiar with a patient's medical history and needs, to continue to direct their care while admitted to the hospital or rehab facility, with coordination of care by other providers and specialists when that is needed. During my rotation, I saw referrals to United States medical centers of excellence in cases of complex diagnoses, to ensure that appropriate treatment options were considered while a plan of therapy was developed. I had not seen this before. The quick availability of the physician to advise patients and answer medical questions is another major advantage of the model of care provided by Premium Medical Home. I have not seen this in other medical clinics. Patients have the option to communicate with their physician using the means they feel most comfortable with, whether it be email, text, phone, or in person, without being limited to the typical M-F 8-5 office hours that most practices keep.
Excellent medical care is provided in a professional manner addressing the individual needs of the patient. I am very grateful for having had the opportunity to work with Dr. Kelly and hope that my patients will be able to benefit from the same model of care in my future practice.
ARTHRITIS PAIN AND WEIGHT LOSS by Robert H. Kelly, MD FACP
We all know the importance of nutrition with regard to diabetes and heart disease. Somewhat less well-known is the role of nutrition in patients with chronic pain. A recent study looked at nutrition with regard to knee pain.
ASPIRIN HAS A ROLE by Robert H. Kelly, MD FACP
Aspirin, a derivative of willow leaf, has had a long relationship with mankind. Ancient Egyptians are said to have used willow bark (basic aspirin is in willow bark) as a remedy for aches and pains. Nearly 3,000 years ago Hippocrates recommended willow to ease the pain of childbirth and to reduce fever. Celsus, the Roman writer, also suggested willow leaf for inflammation.
WHEN TO GET THE FLU VACCINE by Allan R. Kelly, MD FACP
The flu vaccine became available in September. It is not uncommon to hear people say, "When is the best time to get the flu vaccine?" Some people have heard that it is good to wait.
THE SLIPPERY SLOPE by Allan R. Kelly, MD FACP
By now we have all read that physician-assisted suicide is legal in Washington State, Canada, and elsewhere. At PMH we consider this a dangerous stepin the wrong direction. We believe that the dying should be cared for so that they are comfortable every day with their families and those who can help them.
PMH QUOTATIONS FALL 2015
"I will keep the sick from harm and injustice. I will neither give a deadly drug to anybody who asks for it, nor will I make suggestion to this effect."
Hippocrates, a physician, 375 BC
"In every human being there is a special heaven, whole and unbroken."
Paracelsus, a physician, 1527
"All we know is still infinitely less than all that remains unknown."
William Harvey, a physician, 1640
"We need a system that rewards the physician who understands the limitations of guidelines."
George Sarosi, MD, 2015
PMH STORY by Robert H. Kelly, MD FACP
A subscriber had dementia for many years. Her husband was dedicated to her care and made all her medical decisions. Like to many of us, things such as wills and legal documents seemed not as important as being sure that a loved one's needs were met in a timely manner.
The husband died leaving the wife still confined by dementia but without her husband to speak for her. A will had been left but an advance directive or health care power of attorney had never been signed.
The PMH member, nearly 90 years old, was found to have a tumor affecting her brain. The prognosis was hopeless but neurosurgery carried a slim chance for temporary relief. There was no one there to speak for her. There were some remote relatives who were not in a position to make decisions for her.
Dr. Kelly was well-aware of the patient's previous wishes and what her husband had wanted for her. With this in mind, Dr. Kelly asked another physician to consult. Together, the two doctors completed a health directive reflecting the husband's and wife's prior wishes. An appropriate Do Not Resuscitate order and referral to Hospice were made.
Because the PMH physician was familiar with both the patient's and her husband's wishes and desires over the course of years, there was an informed and respectful referral for care which in no way hastened or accelerated the end of her life, but allowed peace and quiet that might have otherwise been out of reach. At such a time, a well-established relationship with a doctor is important.
APPENDICITIS ALTERNATIVE TO SURGERY by Allan R. Kelly, MD, FACP
In 1886 a disease called typhlitis was theorized to be a consequence of appendiceal inflammation and rupture. Over the next 20 years appendectomy was refined. By the 1920's, appendicitis was a surgical emergency treated universally with appendectomy.
CARDIAC ARREST AND BYSTANDER ASSISTANCE by Allan R. Kelly, MD, FACP
We’ve become familiar with the scenes from movies and such of trying to resuscitate someone whose heart has stopped. It is a complex process, and seems like something only doctors and nurses can do. But new research shows that simply pressing on the unconscious person's chest 60 times a minute can make a difference in survival.
CIGARETTE SMOKING AND CHANTIX by Allan R. Kelly, MD, FACP
We have seen the ads on TV for drugs curing serious illness and then comes the long list of side effects, things that might happen if you take the drug. This creates a problem for patients. The doctor may recommend a drug to help them, such as Chantix, but the implied threats in advertisements on TV can overwhelm. Many patients reject use of the drug out of hand based on these intimidating lists of problems. Use is infrequent and there are few friends with experience to share.
DEMENTIA by Robert H. Kelly, MD FACP
In a recent study in the Journal of the American Geriatric Society (August 2014) Joseph, et al show that dementia is not necessarily associated with increased risk of traffic accidents. The author studied 31,000 participants involved in a high blood pressure study. All were community living and not demented. Some had mild cognitive impairment. The results showed a surprising correlation between cognitive impairment and motor vehicle accidents: Motor vehicle accidents decreased with cognitive impairment. No specific measure of driving or accidents per mile driven was made, though those with cognitive impairment were more likely to be infrequent drivers.
SORE THROAT by Robert H. Kelly, MD FACP
Having a sore throat can be uncomfortable. There is risk of bacterial infection, like streptococcus, and antibiotics are appropriate for such disease. Less than 10% of sore throats are caused by streptococcus, so the majority of sore throats do not require antibiotic treatment and are related, principally, to viral infections. Antibiotics can kill strep, and can lessen symptoms of strep throat. But should antibiotics be used for non-streptococcal sore throat? Generally speaking, no.
PMH QUOTATIONS Summer 2015
"Medication and surgery are cornerstones of our efforts to heal patients but honesty and respect…will always be paramount to our success as physicians."
Jesse Raiten, M.D., JAMA, August 4, 2015
"When the doctor really cares about the patient everything else follows; the hard part is to align oneself to care, especially in the face of the often frenzied pace of medicine today."
Michael Khan, MD, NEJM, March 2015
"I have sacrificed my ‘physician-hood’ to document nonsense [in the electronic medical record]. This documentation we do does not benefit our patient in any way. In reality, it just ensures that we are properly reimbursed by the insurance companies."
Hujefa Vora, MD, Tarrant County Physician, July 2015
PMH STORY by Robert H. Kelly, MD FACP
Shoulder and arm pain had troubled a PMH subscriber for a couple of months. With an upcoming special event on Saturday, the problem had become a distraction. She called the office and a referral was made to a specialist for the week after the special event but the pain persisted.
On Friday afternoon, she called for more help. There had not been a visit in many months. Obviously having severe pain, some evaluation was in order. A request was made to meet Dr. Kelly in the Emergency Room the next day. The subscriber did not want to do this because of the amount of trouble sometimes associated with an Emergency Room visit. Dr. Kelly recommended instead that they just meet at the Emergency Room waiting area and then make a decision on whether or not checking into the Emergency Room for further evaluation would be needed.
The new Marion Emergency Care Center at Harris Hospital downtown makes a great place to visit and make a decision about needs. At 8:30, Dr. Kelly met the subscriber and a proper evaluation and examination was done. The problem did not seem to be dangerous at all, and a decision was made to plan x-rays at a later time and begin treatment for what was likely an inflammatory musculoskeletal condition. She did not "check in" to the Emergency Room, saving hours of time and great expense.
Premium Medical Home makes such visits possible. As a PMH patient you are able to see the same physician at the hospital, who will also then see you at his office, the same physician with whom you have spoken on the telephone, whether it is a weekend or a weekday. Because there are fewer patients in Premium Medical Home, there is more time to try to understand the patient's needs and circumstances and try to match the visit or treatment more carefully with these matters of convenience and comfort.
SURGICAL VERSUS NONSURGICAL TREATMENT OF A SHOULDER FRACTURE by Allan R. Kelly, MD FACP
As we get older, fractures become more common and often require surgery. Generally, we are going to leave the decision to have surgery to the orthopedic surgeon. A recent study in the Journal of the American Medical Association (March 2015) by authors from Europe, compared shoulder (humerus) fracture outcomes at six months, 12 months, and 24 months after treatment. These were serious fractures of the proximal humerus with displacement (separation) of the bone fragments. Patients were randomized to non-surgical treatment (sling immobilization) or surgery (fracture fixation or shoulder replacement).
STATINS by Robert H. Kelly, MD FACP
CMedical treatment of disease is meant to promote better health, reduce need for medical care, and allow fuller enjoyment of life. Medical treatment should not promote harmful or high-risk behavior. Statins are used to reduce the problem of disease and death caused by hardening of the arteries. Most importantly, statin drugs, in the appropriate population, significantly reduce the risk of heart attack, stroke, and premature death.
CLOSTRIDIUM DIFFICILE by Robert H. Kelly, MD FACP
C. difficile is a difficult problem in medical care today. C. diff infection can cause diarrhea, severe illness, and even death. Diagnosis is based on testing for the presence of C. difficile organisms in a stool specimen. There are novel treatment ideas out there. A previous PMH@Home article mentioned doing a stool transplant to treat C. difficile. Another idea is to improve identification and diagnosis of disease.
SMART WALKING by Robert H. Kelly, MD FACP
An article in JAMA (Accuracy of Smart Phone Applications, 2/10/2015, Vol. 313, #6, pg. 625), looked at the accuracy of some of the devices used to measure activities or steps. The devices were compared against a standard 500 and 1500 step trial. A treadmill was used set at 3 miles per hour and 10 different devices were worn. Step count from the devices was measured after each trial.
PEANUT ALLERGIES by Allan R. Kelly, MD FACP
Peanut allergies are a problem in the pediatric age group, but I thought PMH members would be interested in a report from the New England Journal of Medicine on how to prevent peanut allergy from developing.
PMH QUOTATIONS Spring 2015
"They who are accustomed to daily labor, although even weak or old, endure labor more easily than the robust or young who are unaccustomed to it."
Hippocrates
"I tell all my patients that frequent exercise is just as important as their medication in controlling their cardiovascular disease."
Joseph S. Alpert, MD
"At day's end, after we have stripped away the science, medicine consists of one person helping another, and the visceral desire to assuage another's hurt, to provide hope even when we have lost it ourselves."
Samir K. Shah, MD
PMH STORY by Allan R. Kelly, MD FACP
Premium Medical Home has many components, including direct communication by telephone and cell phone between the doctor, the patient, and the patient's family. A recent example of the value of direct communication involved an elderly lady whose husband could no longer care for her at home. He spent some time choosing an excellent assisted living facility. He chose one that was close to his home and that offered much of what he wanted. He moved his wife to the facility on a Wednesday. All seemed well, but five days later on Monday, the husband called the doctor with bad news. The facility could no longer care for his wife, and he would have to take her home the next day. He was told her needs were beyond the capacity of the facility because of behaviors the facility could not handle. The PMH doctor asked who had told him that his wife would have to leave and then set up a conference call between the husband, the facility charge nurse, and the physician. In this 3-way conference call, the specific concerns of the charge nurse were explored and discussed. The problem was amenable to medical treatment, and the doctor made recommendations for changes in medication and behavioral modifications. The nurse, the husband, and the doctor agreed on a plan of care over the next several days, and the facility agreed to keep the wife in their facility. Psychiatric consultation was also arranged.
The next day, the charge nurse reported that the behaviors had improved.
Later, the doctor's office received a thank you note from the husband saying he had given up hope that his wife could stay in the facility and was surprised by the quick conference call. He further added that the nurses at the facility much appreciated the prompt assistance.
A doctor's schedule can often be busy or hectic, but less so in a PMH office. PMH emphasizes the comfort and convenience of patients and their families. Comfort and convenience are not trivial, and enhance the experience of patients and families in their medical care.
SLEEP AND WAKEFULNESS by Robert H. Kelly, MD FACP
A recent report showed that of nearly 1000 patients referred to the Mayo Clinic for insomnia, 91% were found to be suffering from obstructive sleep apnea, not from simple insomnia. In such cases, treatment with standard sleeping pills would worsen the sleep apnea problem, the disease which was driving the patient's insomnia: why is this so?
IMPROVING PRIMARY CARE by Allan R. Kelly, MD FACP
Continuous improvement is an important goal. We want to do a better job. One of the great interests in medicine today is to improve the outpatient care of patients with serious chronic illnesses. A recent study looked at how to improve care for high risk and chronically ill children. The study called the process "enhanced medical home." I have reviewed many studies of how organizations can improve care: the results have been so-so. Some added more healthcare practitioners, nutritionists, social workers and consultants. But this study proposed "comprehensive care." The goal was to have the clinic open 40 hours per week and staffed by a physician and nurses. Another big element was: "All patients had the cell phone number to directly reach one of the primary care clinicians at all hours." There were direct conferences with ER doctors about emergency care. These are the same types of interventions that we emphasize in Premium Medical Home.
AMERICAN HEART ASSOCIATION, STATIN USE, AND EXERCISE by Allan R. Kelly, MD FACP
In 2013, the American Heart Association changed guidelines for the use of statins, doubling the number of Americans falling into the "treatment recommended" group.
HAND WASHING by Robert H. Kelly, MD FACP
There are at least two key elements to hand washing: the cleansing agent and the method of drying. The most important disease control for the doctor to do in the clinic, and for patients to do in their everyday lives, is to keep their hands washed at appropriate intervals. This is true for all of us prior to mealtime and after being in the restroom or public places. With adequate hand washing, significant reductions in infectious disease have been reported in hospitals, schools, and elsewhere.
PMH QUOTATIONS Winter 2015
"Most important of all, your patients may not see [things] the same way that you [physicians] do. We [patients] are the experts on what we value."
J.McDonagh, JAMA Internal Medicine, 2014; 174 (12): 1889.
"Walking is man's best medicine."
Hippocrates
"The best preventive approach in frail older adults may sometimes involve doing less rather than more."
M.Clarfield, JAGS 2010; 58: 2019.
PMH STORY by Allan R. Kelly, MD, FACP
The patient was an elderly gentleman whose daughter was his caregiver. He lived in a rural area, and most of his care had been provided by rural doctors. He was hospitalized, and the PMH doctor was asked to visit. During the consultation, staying in touch via a few cell calls, the patient's illness and needs were tracked.
Soon thereafter the patient was discharged home. The patient's daughter requested that the PMH doctor continue to care for her father at home, despite the distance. The PMH doctor asked the daughter what value she saw in this extra cost. She said that after decades of trying to coordinate her father's care, she had never before had the personal cell phone number of a physician. She found it so unusual, so helpful, that even though she might not be able to bring her father to see the PMH doctor on a regular basis, just knowing that she could consult by telephone when needed was valuable to her.
We hope that all doctors will embrace the idea of direct, open, and convenient communication between themselves and their patients. As our motto says, it's "like having a doctor in the family.", a doctor you can call when you need to, when there are questions, and when there is illness. A direct relationship can promote better outcomes for patients and their families.
Of course, there will always be limits. Doctors need to sleep and have time to do their work. But it is not a burden to offer the same direct communication to our subscribers as we would to family, neighbors, or old friends. This is part of the PMH subscription, a premium valuable to patients and families.
ANXIETY, EXERCISE, AND YOGA by Allan R. Kelly, MD, FACP
Researchers reported on the effect of exercise on anxiety. Participants in the study were randomized into three groups. One group would only stand, another would walk, and the third would jog gently or walk quickly on a treadmill for ten minutes.
NUTS, CORN, AND POPCORN IN DIVERTICULOSIS by Robert H. Kelly, MD, FACP
Diverticula, or the little pouches that form along the wall of the colon, measuring from a few millimeters to 2.0 centimeters in size, are part of aging. Rarely seen before the age of 40, by the age of 70 they are common. They are a normal part of the colon after the age of 60, a condition called diverticulosis.
EXERCISING FOR HEALTH by Allan R. Kelly, MD, FACP & Robert H. Kelly, MD, FACP
Exercise improves health. Recent reports continue to confirm that sedentary adults over the age of 50 have a fourfold increased risk of death over the course of study compared with adults who pursue moderate physical activity.
FOOTBALL SEASON by Robert H. Kelly, MD, FACP
Data were published several years ago looking at NFL football players’ cardiovascular risk factors. Compared to the normal population of average risk individuals, men 25-37 years of age, there were some striking differences that suggested football players were an unhealthy lot: body mass index was higher, waist size higher, and blood pressure higher.
PMH QUOTATIONS Fall 2014
"The fact is that in order to have the privilege of doing this job, we may have to miss dinner once in a while to take care of someone who got sick. . ."
Victoria Johnson, MD, NEJM 2013; 369:2279
". . . the relief and comfort given to an aged patient often effect the prolongation of life if only by restoring the willingness to live."
Alfred Worcester, MD, JAMA 2014; 312:1159
PREMIUM MEDICAL HOME STORY by Allan R. Kelly, MD FACP
Mr. Doe had excellent health most of his life, but had recently been having abdominal symptoms. Workup showed an unusual malignancy.
We made arrangements for consultation in Fort Worth. The patient was satisfied with the oncologic consultant, and we began a plan of treatment. But the patient was uncertain whether or not more should be done. The oncologist was a new doctor for Mr. Doe who didn’t know entirely how to "read" the doctor's manner.
This led to repeat telephone consultation with his PMH doctor. The patient was trying to develop insight into the consultant's style. The PMH doctor had known this consultant for decades, understood these issues, reassured the patient, and went over the details. Though helpful, the patient wanted more. Fifteen years earlier, for a malignancy that had been cured, he had ended up going to M.D. Anderson hospital. He wondered if he should go back.
The patient was getting ready to go on vacation, was anxious, and faced a potentially life-threatening illness with important decisions to be made. After hanging up from Mr. Doe, Dr. Kelly called M.D. Anderson and found the names of two doctors there who treated this specific malignancy. One of the doctors kindly and promptly called back. Dr. Kelly was able to review what M.D. Anderson could do for Mr. Doe. The M.D. Anderson doctor offered to see Mr. Doe at a time of convenience.
Dr. Kelly called back Mr. Doe. Dr. Kelly outlined what he had learned about what M.D. Anderson had to offer. Mr. Doe listened carefully, considering his options. He said that he would think about it some more, that he appreciated Dr. Kelly's work, and it sounded to him like he would probably decide simply to stay right here in Fort Worth and work with his new oncologist.
When patients face severe issues, such as cancer, there are going to be a lot of questions. Many of those questions should be answered and should be resolved by the oncologist. But there will be issues of personality, manner, and judgment calls where an open, friendly, and professional relationship with a physician can make a big difference. But also, does the primary care doctor have time to search out answers and options for his patient? In many practices, driven by volume, short appointments, and insulation of the physician from telephone contact with patients, there may not be enough time. In the PMH practice, it is our commitment to make that time available to you at times of stress such as an important diagnosis, injury, or hospitalization.
THE IPHONE PANCREAS by Allan R. Kelly, MD, FACP
Diabetes is a major cause of illness and expense in the United States. Its complications include amputation, end-stage renal disease, stroke, and blindness. Diabetes for centuries was treated with dietary modification, weight loss, and calorie restriction. Since 1928, the development of insulin and the ability to easily measure blood glucose have transformed the lives of diabetics for the better.
OSTEOARTHRITIS PHYSICAL THERAPY by Robert H. Kelly, MD, FACP
A series of recent publications have examined the safety of "hypnotic" drugs, drugs like Ambien, Xanax and Ativan. This class of drugs is derived from Valium. They have been helpful in medical practice. Ativan, for example, has been used to treat anxiety, seizures, sleep disorder, and psychosis.
OBESITY by Robert H. Kelly, MD, FACP
Nutrition is good but too much food, eating more than we should, can cause obesity. Obesity leads to diseases such as sleep apnea and liver dysfunction, and it makes other diseases worse, like hypertension and diabetes mellitus. Obesity increases weakness, sickness, and risk.
ADVERSE EFFECTS OF MARIJUANA USE by Robert H. Kelly, MD, FACP
Though Colorado has made marijuana purchase and possession legal, there is debate about whether or not marijuana is harmful. It's a safe bet that it is: medicines which adversely affect judgement and health, create dependency and habituation, and do not improve health are bad and should not be used.
PMH QUOTATIONS Summer 2014
"Above all, physician do no harm must be first and foremost, just in front of humility."
Peter Weiss, MD, FACOG, UCLA School of Medicine, 2014
"For a generally healthy 85-year-old, the physical exam could reasonably be limited to blood pressure measurement and assessment of the body mass index."
Michael Rothberg, MD
"The opportunity for doing wrong by careless talk to sick people and their families seems almost limitless."
Sol Pepper, Doing Right, p.26
PREMIUM MEDICAL HOME STORY by Robert H. Kelly, MD, FACP
The patient received a note from his pharmacy supplier that a critical brand name medication would no longer be covered. Early in the course of his illness, he had been unable to tolerate the generic version of the medication. The brand name was well tolerated and for 10 years had helped prevent serious illness. In addition, recent gastrointestinal complications had increased the risk of medication side effects. The patient came by the office to address concerns about changing medications.
Prior to the patient's arrival at the office, Dr. Kelly had received information about the denial of medication coverage. A form had been completed requesting pre-authorization for the questioned medication. In the meantime, thought was given to whether or not a change in dose or change in medication would be acceptable.
Dr. Kelly called a neurology specialist. The specialist answered the call and said that he would be happy to see the patient in 15 minutes. A quick consultation was completed. The specialist thought it best not to change the medication or dose. We communicated these conclusions to the insurance company, and the needed medication was then authorized.
In the course of an hour, a serious question had been addressed, pre-authorization completed, and consultation done to confirm the course of treatment. This level of coordination is accomplished on a daily basis in many medical offices, but because of often crowded schedules, communication may be delayed. In large offices, different providers are tasked with different elements of the care, contributing to fragmentation of care and possible delay. In the Premium Medical Home, however, more often the physician and the patient will directly address and resolve these questions, promoting more rapid and less complicated resolution.
This is one of the benefits of a Premium Medical Home, providing not only for prompt medical care and recommendations, but also for the patient's convenience and comfort.
DO PHYSICIAN EXTENDERS IMPROVE MEDICAL CARE? by Allan R. Kelly, MD, FACP
A report in the February 2014 Journal of the American Medical Association addressed whether adding more money and using physician extenders can improve medical care. The study, done in Pennsylvania between 2008 and 2011, looked at practices run by doctors based on their own judgment versus practices participating in a government designed program. The interventions in the latter group included bureaucratic creations like "breakthrough series learning collaborative," "monthly quality indicator reports," "practice coaches," NCQAPPC-PCMH recognition with level one recognition required, and performance improvement efforts. More definitively, the Pennsylvania experiment offered doctors money, a bonus of up to $95,000 to each physician who hired a physician extender such as a nurse practitioner or physician's assistant.
AMBIEN, XANAX, ATIVAN… by Allan R. Kelly, MD, FACP
A series of recent publications have examined the safety of "hypnotic" drugs, drugs like Ambien, Xanax and Ativan. This class of drugs is derived from Valium. They have been helpful in medical practice. Ativan, for example, has been used to treat anxiety, seizures, sleep disorder, and psychosis.
MARION EMERGENCY CARE CENTER by Robert H. Kelly, MD, FACP
Harris Hospital has opened the new Marion Emergency Care Center and an attached Senior Health Center. Until the opening of the Marion Emergency Room, Harris's ER was plagued by crowding, hallway examinations, and long delays. These have been eliminated with the new Marion ER. The whole hospital seems to have refocused on the comfort and dignity of sick patients and their families while continuing to provide medical care.
COLON CANCER SCREENING by Robert H. Kelly, MD, FACP
The American Cancer Society recommends colon cancer screening after age 50. Cancer screening is commonly done either with fecal occult blood testing or colonoscopy. The American Cancer Society prefers colonoscopy because it is a more thorough exam. But despite being better, this recommendation causes some harm: recommending colonoscopy and neglecting the option of the stool test kit reduces the overall level of screening.
PMH QUOTATIONS Spring 2014
"The needs of the patient come first."
Mayo Clinic
"Where the art of medicine is loved, there is also a love of humanity."
Hippocrates
"That which is used develops. That which is not used wastes away."
Hippocrates
PREMIUM MEDICAL HOME STORY by Robert H. Kelly, MD, FACP
The patient, a doctor, had been well, but suddenly became ill on a Sunday afternoon. There was no recent travel, and others in her family were well. She suffered marked nausea and repetitive vomiting: nothing would stay down.
When she called, she reported to her doctor that she had tried a dose of nausea medicine: even that would not stay down. She felt as bad as she had ever felt in her life. She told her PMH doctor she was going to the emergency room.
After hearing the story, her PMH doctor asked a few questions. There was no sign of fever or bleeding. She had never been sick like this before. Options were discussed. Recommendations were made to rest and to take a second dose of the anti-vomiting medication, try some clear liquids, call back after half an hour and delay going to the ER.
At the time of her call back, she was resting in bed. She had taken the extra dose of medication and had kept down some sips of clear liquids. She felt better and decided not to go to the emergency room after all. The evening was spent in the peace and quiet of her own home, not at the ER. Her body was able to recover somewhat more naturally, with the help of the medication.
The next morning she reported recovery and decided to go on to work. This was, in short, an episode of food-borne illness with nausea and vomiting which resolved.
An experienced doctor who picks up the phone can give a person, even a fellow health care provider, confidence and prudent advice she can follow. Too often telephone calls to a doctor's office after hours are handled differently: the answering service, the waiting, the nurse who triages the call and the customary, "If you are suddenly ill, go to the emergency room" are routines that have to be followed. At PMH we think it is better when a knowledgeable, committed physician answers the phone. Familiar with the member's history, her health, and the tools available, the doctor can make a more defined, personal set of recommendations.
Sometimes patients are sick and have to go to the ER or hospital. But in many cases, knowledge and experience quickly accessed can save a trip to the hospital or emergency room. This is one of the benefits of the Premium Medical Home model.
NUTS AND HEALTH by Robert H. Kelly, MD, FACP
"You are what you eat", our grandmothers told us. Diet is important. Nut consumption has been of interest to doctors and patients. Are nuts good for your health? This question was addressed in the 2013 New England Journal of Medicine study of 100,000 men and women in the Nurses’ Health Study from 1986 to 2010. That was 3,000,000 years at risk that were assessed! The recent study showed that nut intake correlated with survival. Pooled analysis for death showed a 7% risk reduction for those who ate nuts less than once a week on average, compared to those who did not eat nuts; 11% risk reduction for those eating nuts at least once a week; 20% reduction for those eating nuts 7 or more times per week. Eating nuts at least once per week appeared to reduce overall mortality, and specifically mortality related to cancer, heart disease and respiratory disease.
AROMATHERAPY by Robert H. Kelly, MD, FACP
Falls in the elderly can lead to severe injury, increased risk of death and loss of independence. Efforts at reducing falls have attracted attention for some time in geriatric care, especially in hospitals and nursing homes, where the elderly are at high risk of falling.
TAKE YOUR MEDICINE by Allan R. Kelly, MD, FACP
One of the critical jobs a physician faces is to identify disease and propose treatment that will alleviate suffering and promote health. Oftentimes, medications are an important part of this effort.
SHINGLES VACCINE by Allan R. Kelly, MD, FACP
The shingles vaccine, Zostavax, has markedly reduced the incidence of painful shingles. This is a boon to adults. The vaccine was originally released for the over 60 population, and then later approved for over 50. At a December meeting of the American Advisory Committee on Immunization Practices, the CDC addressed the relative benefits of vaccinating at 50 or at 60.
PMH QUOTATIONS Winter 2014
"The health of my patient will be my first consideration."
Declaration of Geneva, JAMA, November 27, 2013; Vol. 310, No. 20: p. 2191
"I don't know what your destiny will be . . . but I know one thing: the only ones among you who will be really happy are those who have sought and found how to serve."
Albert Schweitze
"The only real change, it seems, is that every year, fewer of us practice medicine and more of us talk about it."
James H. King, MD, Annals of Internal Medicine, January 7, 2014; Vol.160, No.1: p. 68
PMH STORY by Allan R. Kelly MD FACP
The elderly patient had not been seen for some time in the doctor's office. He had three children. There had been no complaints from the patient, nor had the doctor received any calls from the family.
A call came in from the patient's daughter who lived far away. She asked the doctor to call her back.
When time allowed, the doctor called. At first the daughter's concerns seemed minor. She talked about her father's weight gain and then his poor spirits after the death of the mother a year ago. But with time the daughter talked about other concerns. She recalled her father's tremor and a fall months ago which had not been reported to the doctor. The patient and doctor visited the next day. With special attention to the fall, adjustments were made in medication and arrangements made for physical therapy to address imbalance and fall risk.
Allowing time for conversations like this results in better understanding. There is no way to predict what we will learn from a conversation. A doctor needs time to allow families to bring their concerns forward. In a practice driven by volume and billing codes, such time is hard to come by. In a practice where families communicate indirectly with the doctor through office staff, there is less opportunity for direct dialog.
In Premium Medical Home, we are committed to making time for family members to talk to the doctor. The doctor will, of course, respect the patient's privacy. The relationship is direct: the patient or family talk directly to the physician when they feel the need. The number of patients is limited so that there is time to talk. This is a part of Premium Medical Home.
STATIN DRUGS MAY PREVENT DEMENTIA by Robert H. Kelly, MD, FACP
The FDA, in the last year, warned that statin drugs might be associated with memory problems. Are statin drugs bad for our brains? We don't see such evidence.
For example, a recent study published in the Journal of the American Geriatric Society (2013, Volume 61) showed using statin drugs before Alzheimer's disease develops may reduce the risks of developing Alzheimer's.
SORE THROAT, COUGH, AND BRONCHITIS - WHAT TO DO? by Allan R. Kelly, MD, FACP
Most of us have had wintertime illnesses characterized by stuffiness, drainage, sore throat, and cough. For example, see the PMH Story in this newsletter. The majority of these illnesses will resolve spontaneously and antibiotics usually make no difference
There are things we can do. Websites can be informative (e.g., MayoClinic.com). For adults, over-the-counter medications can be helpful. Tylenol, zinc lozenges, and vitamin C have all been shown to be useful for some patients. Even the old home remedy of a teaspoon of honey reduces nighttime cough and discomfort. Prescription medicines also may slightly reduce symptoms.
FRAILTY by Robert H. Kelly, MD, FACP
As we age, our health changes. And there is a pattern - some are healthier and others are not. A syndrome of chronic poor health in the elderly is called frailty.
Frailty is a syndrome, a collection of symptoms and signs of illness of uncertain cause. The key elements of frailty are: loss of function in an activity of daily living, decreased strength or energy, unintended weight loss, and increased vulnerability, infection, and illness.
SHOULD I MEASURE MY OWN BLOOD PRESSURE? by Allan R. Kelly, MD, FACP
When high blood pressure is identified and treated, there is a substantial immediate and long-term reduction in the risk of stroke. Office measurement and treatment are the bedrock for the evaluation and management of hypertension.
Blood pressure can be easily measured in our homes. Blood pressure monitoring equipment is available in pharmacies and health clubs. Does self-monitoring of blood pressure further reduce the risk of stroke or heart attack compared to simple office measurement?
HEPATITIS C by Allan R. Kelly, MD, FACP
Hepatitis C is an uncommon but dangerous infection. Those who have had transfusions are at greater risk. It can result in problems including cirrhosis, liver cancer and death.
Hepatitis C spread throughout the world after the Second World War.
PMH FEES
New PMH fees will go into effect on January 1, 2014. The new fees are posted on our web site,www.PremiumMedicalHome.comand are also available by calling the office. As your PMH renewal becomes effective, you will be billed for the new 2014 fees.
PMH QUOTATIONS FALL 2013
"Our dean asked the medical students how many of them had been advised by at least one physician not to go into medicine; 80% of the students raised a hand."
- Lawrence Hergott, MD ; "The View From Fiesole"JAMA, July 10, 2013; Page 147
"I have the distinct feeling that the patient in America is becoming invisible. She is unseen and unheard. . . I generally insist that we go to the bedside, but that is often the place where the team is no longer at ease. I realize what has happened: the patient in the bed is merely an icon for the real patient, who exists on the computer."
- Abraham Verghese, MD; JAMA, July 17, 2013; Page 265
"To prevent disease, to relieve suffering, and to heal the sick - this is our work."
- William Osler, MD
PMH STORY by Robert Kelly MD FACP
The patient was at home. Her husband had died some years ago. Her family lived out of state.
She noticed a strange feeling in her chest. Heart attack was far from her mind – there was no prior problem with heart disease. Simple remedies like yawning and deep breathing did not resolve the sense of oppression across the chest. She called her Premium Medical Home doctor's office at approximately 9:00 a.m. and was immediately speaking with the PMH nurse so well known to her. Within minutes, her PMH doctor had reviewed her chart and her problem, and recommendations were given to go to the hospital for care. The doctor called and alerted the hospital staff to the patient's needs.
A cardiologist, whom the patient had not previously met, was waiting when the ambulance arrived. By noon, cardiac catheterization and intervention was done. The problem was identified, a solution provided, and she was soon recovering in the intensive care unit.
Lying on a bed in the ICU, surrounded by strangers, there was a certain feeling of anxiety and anonymity. At 2:00 p.m., the patient's PMH physician came to see her. On his arrival, the patient exclaimed, "Oh, Dr. Kelly, I can’t tell you how good it is to see you." Discharge was made several days later, with a continued healthful life at home.
This is a Premium Medical Home story, not because of a favorable medical outcome, an outcome which would have likely been achieved with prudent care. What is different is that, in the midst of this illness, in the midst of all the new people, and in the midst of the intensive care unit, members of a Premium Medical Home can count on seeing the physician whom they have learned to trust and whose manner and methods they have become accustomed to. They are seen by a physician who knows them and their family, who knows what has been important to them over the months or years prior to their acute illness and who knows the consultants and the hospital staff. This was why the patient was so happy to see her doctor. This is another reason we created Premium Medical Home.
A DOCTOR'S OFFICE VISIT IS NOT ALWAYS NECESSARY by Robert H. Kelly MD FACP
Recent issues in the abortion debate may unexpectedly shed light on efficiency that could improve medical care. The doctor's office is not always the best place to get the medical care we need. Certainly, many treatments are now available without prescription, such as over the counter medications, even the Plan B contraceptive that can be sold to any girl regardless of age. It seems reasonable to ask, if regulators believe a 12 year-old girl has adequate judgment to buy Plan B, why should not a 42 year-old mother of three have the ability to buy antibiotics for her children? This issue of patient directed care deserves attention in less controversial areas.
PHOTOGRAPHS by Allan R. Kelly MD FACP
A helpful communication is taking and sending photos by cell phone. Recently a middle-aged woman noticed a spot on her finger and wondered whether it was the sort of thing that she should check with the doctor. She had hurt it, it was tender, and she thought it was infected. She called my office late in the afternoon. She asked whether or not she should go to the emergency room.
SHELF LIFE: BETTER THAN YOU MIGHT THINK by Robert H. Kelly, MD FACP
The question often arises: how long after the expiration date can the medication still be safely used? From the safety perspective, the answer may be that there is little safety concern, but from a potency or effectiveness perspective some medications do lose their effectiveness. A study was done last year that looked at medications that were held in a federal program of strategic reserve. These medications had expired between 28 and 40 years before testing. Capsules or tablets from each medication were tested looking for the presence and concentration of the active ingredients.
REFLUX MEDICINES AND FRACTURES by Allan R. Kelly MD FACP
The longer medicines are on the market the more we learn about their benefits and their risks. Learning about the risks of medicines can clarify how best to use them safely. Newly reported problems with proton pump inhibitors (PPI's) have come to light after twenty years of experience. Examples of PPI's are Nexium, Prilosec, omeprazole, Protonix, and Prevacid, among others. They often relieve symptoms of reflux and protect from complications such as ulcers, perforation and bleeding. They do a great job. It appears that prolonged use of PPI's increases the risk of fracture. This is important as fractures are associated with serious health problems, surgery and functional loss.
DEMENTIA: MEMORY OR BEHAVIOR? by Allan R. Kelly MD FACP
We all know that smoking causes suffering from stroke, heart attack, and cancers. There are other risks worth being aware of, as we counsel family and friends who smoke.Tobacco use correlates with psychiatric illness, complicates its treatment and contributes to early mortality and morbidity in those with mental illness. This is a perspective that many may be unaware of.
PMH QUOTATIONS SUMMER 2013
""Once with his patient, he must, in word and thought, attend to nothing but his patient's case and what concerns it."
" - Oath of the Hindu Physician, circa 1500 B.C.
"Under the present system of supervision it is unlikely that many of the successful surgical innovations we have witnessed would have been achieved "
- Allen B. Weisse, M.D.; Proceedings; Baylor University Medical Center; July 2013, Volume 26, No. 3, Page 310
"". . . the importance that professionals ascribe to patients' deep experience and such enduring moral practices of caring, as the laying on of hands, the expression of kindness, the enactment of decency, and the commitment to presence – being there for those who need them. This is the embodied wisdom medical students need to learn and we all must remember."
- Arthur Kleinan, M.D.; New England Journal of Medicine; April 2013
PMH STORY by Robert R. Kelly, MD FACP
Around 2 PM one weekday afternoon, a long time patient e-mailed Dr. Kelly with concerns about depression and anxiety. An hour or so later, looking at e-mails while between patient appointments, Dr. Kelly noted the message. The chart was pulled for Dr. Kelly, who sent the patient a quick e-mail that discussed some principal treatment options to consider, including a change in medication, visits, consultation, and further testing. Within minutes, an opportunity arose to call the subscriber on the phone; discuss symptoms; review the e-mail notes; and establish reasonably that there was no suicidal risk. Options were discussed.Based on the patient's preferences, a referral was made to a counselor. The Premium Medical Home nurse called the subscriber back that afternoon with contact information for the counseling.
Though happy to visit with the subscriber at an office visit, the needs, in this case, were well met by a consideration of the patient's symptoms; review and modification of treatment; and referral to an appropriate source for psychological counseling.
Subscribers can avoid long waits for a return call when they are in a Premium Medical Home. They do not need to first talk to a nurse or a nurse practitioner. There is no need or expectation that they visit at the office to receive information about options or alternatives, as some of the most important care given to patients occurs on the phone and when they are at home.
Your Premium Medical Home subscription recognizes this fact and creates avenues for you to contact your doctor directly for advice, counsel, treatment, and referral where needed. This leads to more efficient care and better satisfaction.
HOSPITAL ACQUIRED INFECTIONS: NOT ALL SOAPS ARE THE SAME by Dr. Allan R. Kelly, MD FACP
Everyone knows that antibiotics can have side effects, and one of the side effects can be diarrhea. Many have heard about Clostridium difficile or C. diff. A disease that is a complication of antibiotic therapy, C. diff can be dangerous, and even a cause of death. The treatment is only partially successful: many patients relapse, some die, and many may face months or years of recurrent illness.
FALLING by Dr. Allan R. Kelly, MD FACP
Falls are embarrassing and can be dangerous. It is important for doctors, patients, and families to work together to reduce falls. After age 70, the most common causes of accidental death are injuries sustained in a fall. Most falls do not result in injury, and it is estimated that people over age 85 will have two to three falls per year.
QUALITY OF CARE by Dr. Robert Kelly, MD FACP
One pernicious element of centrally planned medical and surgical care is an assumption that normal people are not capable of making judgments about what is best for themselves. Can a federal agency better identify what is best? The problem with this assumption was recently demonstrated in a study of weight loss surgery, also called bariatric surgery. The best approach to weight loss in the obese is life style change.
BLOOD PRESSURE by Dr. Robert Kelly, MD FACP
For blood pressure, the doctor should treat the person, not the number. In the younger elderly, those below 80 years of age, treatment of hypertension helps reduce the problem of heart failure, dementia, and stroke. New research on high blood pressure in those older than 80 is yielding surprising conclusions. A recent report from the Netherlands published in The Journal of the American Geriatric Society explores high blood pressure in the over 85 group.
PMH QUOTATIONS
"What is allegedly true and useful today may be shown to be worthless tomorrow."
- Joseph Alpert, MD, The American Journal of Medicine, February 2013
"We medical people really have no idea what we put patients through."
- Edward Viner, MD: The Physician as Patient, 1985
"May there never arise in me the notion that I know enough, but give me the strength and leisure and zeal to enlarge my knowledge. Our work is great and the mind of man presses forward forever."
- Maimonides, physician (1135 – 1204)
PMH STORY by Robert H. Kelly, MD FACP
The patient woke up Friday morning with poor appetite, weakness, diarrhea and vomiting. He spoke on the telephone with his PMH doctor, who suspected a GI virus and prescribed medicines to help with the nausea. In a follow-up phone call the patient was not improved. The doctor recommended admission to the hospital for testing, IV fluids and better symptom control.
The doctor called the hospital and reserved a room for the patient. Initial orders for care were given. The PMH nurse called the patient back with room number and explanation of the admission process. An ambulance was called for transportation.
The paramedics took him to the hospital. The Emergency room was crowded, full of influenza cases and Friday Emergencies. The patient reported that patients were lined up two deep in the hallway, and some family had prepared pallets on the floor to sit or rest.
The paramedics told the ER desk clerk that the patient had been directly admitted to the hospital by Dr. Kelly, and was not to be seen in the ER. The clerk confirmed the bed assignment and the patient went upstairs for continued care. The stay in the emergency room was less than five minutes.
Upon leaving the ER, the paramedic told the patient, "You must have some kind of doctor." His partner added, "Yeah, most of the time when people tell us that admission was arranged by the doctor, no one in the ER knows anything about it so they stay in the ER."
Sometimes emergency room care is necessary and cannot be prudently bypassed. Sometimes the patient's needs are better met in a regular hospital room, not in the Emergency Room. When that is the case, it is good to have a doctor that you can call directly and who will arrange direct admission to the hospital without an unneeded visit to the ER. This is one value of a PMH subscription.
LABORATORY TESTS: TO FAST OR NOT TO FAST by Allan R Kelly MD FACP
In the 20th century, the diagnoses of diabetes and cholesterol abnormalities were based upon fasting blood work. Fasting blood work dates back to the 1930's and 1940's when treatment for diabetes with insulin first became available. A fasting oral glucose tolerance test was the gold standard. Subsequently, fasting was thought to be the appropriate time to test other metabolic parameters. Our patients who were born prior to 1960 are accustomed to the idea that blood work should be taken prior to the first meal of the day.
URINARY TRACT INFECTIONS: OVER-TREATMENT CAUSES PROBLEMS By Allan R. Kelly, MD FACP
Urinary tract infections are a common problem in both the healthy and the frail populations. Traditionally, a urinary tract infection is diagnosed when people have bladder symptoms and laboratory testing shows inflammation of urine, as well as a positive culture. Many are familiar with this scenario in ourselves and our family. We know that a few days of antibiotics will generally take care of the problem.
FLU VACCINATION by Allan R. Kelly, MD FACP
We have all gotten used to the idea that the flu vaccine is good. Most medical organizations recommend routine annual flu vaccine for certain groups. However, past recommendations have generally not included the healthy adult between the ages of 20 and 50.
GERIATRIC ISSUES by Robert H. Kelly, MD FACP
Aspirin keeps attracting attention, some of it negative, some positive. For example, in persons suffering adult ‘wet’ macular degeneration, aspirin use may increase bleeding complications. If you have adult "wet" macular degeneration, ask your eye doctor if aspirin should be stopped or continued. On the positive side, in persons with heart disease or who have suffered stroke, the benefit of aspirin is well proven.
SLEEPING, VITAMINS AND FRESH AIR by Robert H. Kelly, MD FAC
Sleeping pills for insomnia are coming under increasing scrutiny and regulation. Each person deserves careful consideration of the causes and possible treatments for sleep disorder. There is some information that may be generally useful.
PMH QUOTATIONS WINTER 2013
"I hope physicians will avoid words like health care provider and consumer. We are physicians and we care for patients. Let the cost accountants provide and consume."
- Sol Papper, Doing Right: Everyday Medical Ethics, 1983, p. 66
"[Patient] Autonomy is not threatened by hearing the thoughtful opinion of experts about what they claim is the best course of action."
- Arthur Caplan, Mayo Clinic Proceedings, November 2012, p.1041
PMH STORY by Allan Kelly MD FACP
A PMH subscriber had a visitor. His family was hosting a teacher from China. Unfortunately, on the day prior to leaving Fort Worth, there was an accident. The host family's automobile was hit by another car. The car was drivable, and no one complained of injury. Initially, the teacher felt fine. On the way home, he said perhaps he should see a doctor.
Due to leave the next day, there was little time to make an appointment. The obvious alternative was to go to the emergency room, with expected long delays and high bills.
The subscriber called Dr. Kelly. After talking, Dr. Kelly offered to come to the subscriber's home and assist with evaluating and giving recommendations for care.
The visitor, now a patient, was seen and examined. The history was relatively benign, suggesting a whiplash like discomfort in the neck. Physical exam was normal. The medical options were straightforward and outlined to the patient. Symptomatic care was provided. Then the patient said he would need a certificate to give to his physicians in China.
Inquiring into more details, it was determined that a certificate could be quickly provided in longhand writing to satisfy the young man's needs. He returned to China the next day, "certificate" in hand!
The total time involved in this service was less than an hour, as opposed to the many hours that would have been required for an emergency room visit. The availability of medical evaluation and treatment access, which respects the individual's schedule, needs, and pocketbook, is one of the features and benefits of a PMH subscription.
PROVIDING CARE: THE WORK NO ONE SEES by Allan R. Kelly MD FACP
Though the United States continues to have good medical care for its citizens, there are issues that we need to address to improve quality of care and service. We hear people complain about short doctor visits and impersonal care. On the other hand, people are generally confident that the doctor is doing a good job.
RETHINKING THE ASSOCIATION OF HIGH BLOOD PRESSURE AND MORTALITY IN ELDERLY ADULTS by Allan R. Kelly MD FACP
Identifying and treating hypertension is a cornerstone of care for many adults. Over the past 20 years, mortality rates from cardiovascular disease have declined in part because of the power of antihypertensive therapy.
But later in life, the meaning of hypertension becomes more complicatd.
GERIATRIC CARE by Robert H. Kelly MD FACP
Geriatric medicine involves the treatment and care of adult patients with chronic illnesses and functional decline. Fifty percent of older adults have three or more chronic medical problems such as diabetes, arthritis, heart disease, and malignancy. Illness and treatment, combined with advancing years, are associated with decline in a person's function. It is the balance of medications, illness and function that concerns the geriatrician.
ORGANIC FOODS by Robert H. Kelly MD FACP
Some interesting findings about organic food have been reported recently. Research published regarding organic food came in the September 2012 Annals of Internal Medicine. Some of the key findings were:
1. Pesticide levels in urine were lower in children on diets with organic food, although in both regular food and organic food, pesticide levels were well below limits of toxicity.
PRAVACHOL, STATINS, AND MEMORY IMPAIRMENT by Robert H. Kelly MD FACP
Statin drugs are effective at preventing recurrent myocardial infarction. Regular use of statins by those with cholesterol elevation leads to reduced death rates.
Earlier this year the FDA warned about reported memory impairment in statin users: "Cognitive brain related impairment, such as memory loss, forgetfulness, and confusion, has been reported by some statin drug users." The FDA's concern began when several persons taking statin medication wrote the agency about problems with memory that occurred during their treatment.
PMH QUOTATIONS Fall 2012
"In this work against sickness we begin not with genetic or cellular interactions, but with human ones.
" - Atul Gawande, M.D., BUMCP, Volume 25, No. 1, January 2012, Pg. 60
"We miss more by not seeing than we do by not knowing."
- William Osler, M.D. 1926
PMH STORY by Allan Kelly, MD FACP and Robert Kelly MD FACP
Our father, Gordon Kelly, started a practice in Fort Worth in 1953. Over the next 40 years, he served the citizens of our community, the hospitals, and his colleagues in caring for the sick and providing good advice to the healthy.
Gordon's practice was devoted to private and one-on-one care of the individual. This represents an ancient and honorable tradition dating back to the days of Hippocrates. Over time, this basic relationship between a physician and a patient, a unique and personal relationship, has been the basis of medical and surgical care into the modern era.
Up to this point, it has not been demonstrated that there is something better than this traditional relationship. We hope that the development of medical teams, managed care, and diffusion of responsibility will be helpful and beneficial to our fellow citizens and our colleagues, but the benefit is uncertain.
Gordon died on June 29, 2012. His career is the basis of Premium Medical Home. His practice of medicine illustrates the ancient, honorable, and enduring human relationship between the sick and their physician. This is a tradition we treasure and promote at PMH.
CANCER SCREENING AND CONTROVERSIES by Allan R. Kelly MD FACP and Robert H. Kelly MD FACP
There are controversies in the areas of cancer screening. Two controversies emphasize reducing the frequency and intensity of cancer screening in otherwise healthy and vigorous people.
First, the annual visit for women for cervical cancer screening is changing. Years ago the American Cancer Society and the United States Preventative Services Task Force (USPSTF) recommended reducing pap smears to every three years. The recommendations changed as of 2012 to as little as every five years for women over 30.
RETHINKING THE ASSOCIATION OF HIGH BLOOD PRESSURE AND MORTALITY IN ELDERLY ADULTS by Allan R. Kelly MD FACP
Identifying and treating hypertension is a cornerstone of care for many adults. Over the past 20 years, mortality rates from cardiovascular disease have declined in part because of the power of antihypertensive therapy.
But later in life, the meaning of hypertension becomes more complicatd.
CONTINUITY OF CARE IS GOOD by Allan R. Kelly MD FACP
Patients like having the same doctor for a long time, a doctor who knows their medical history well. But does this actually improve outcomes; does it improve efficiency, cost, or morbidity?
The Mayo Clinic has used hospitalists for its inpatients for some time. A recent study, published in April 2012 by Chandra et al., looked at continuity of care among hospitalists and how it affected length of stay, healthcare costs and other outcomes. In one group, the same doctor remained in charge for the patient's hospital stay. In the other group, the attending changed with every shift.
TELE-MONITORING OR PERSONAL COMMUNICATION? by Allan R. Kelly MD FACP
The scientific method involves creating hypotheses and then doing experiments to test the hypotheses. An example of this simply involves the question of how we take care of people as they get older and suffer complex illness. A study in the Archives of Internal Medicine looked at patients over the age of 60 who are at high risk for re-hospitalization because of chronic medical illness. Does increased screening or monitoring improve health?
NOT ALL SYMPTOMS ARE WARNINGS OF DISEASE by Robert H. Kelly MD FACP
Some symptoms are common in healthy people. Hunger, thirst, sleepiness are universal experiences. Symptoms found in more than 30% include nausea, muscle pains and aches, and anger. Fifteen percent of normal persons report difficulty sleeping, headache and head pains, tiredness or lack of energy, nervousness, feeling of tension, worry and dizziness.
SMOKING by Robert H. Kelly MD FACP
We all know that smoking causes suffering from stroke, heart attack, and cancers. There are other risks worth being aware of, as we counsel family and friends who smoke.
Tobacco use correlates with psychiatric illness, complicates its treatment and contributes to early mortality and morbidity in those with mental illness. This is a perspective that many may be unaware of.
PMH QUOTATIONS SUMMER 2012
"The physician must have two special objects in view with regard to disease, mainly, to do good or to do no harm
" - Hippocrates Epidemics
"I love technology, but I think we are discovering that the physician-patient relationship is timeless. It cannot be abandoned . . "
- Andrew Verghese, MD, New England Journal of Medicine, May 17, 2012
"On a lot of patients, we cannot make the correct diagnosis. Some we diagnose, we cannot cure. But there is never a time in the practice of medicine that you can’t be kind to a sick man."
- Tate Miller, MD; BUMC Proceedings, Volume 25, No. 3, July 2012, Page 256
PMH STORY by Robert H. Kelly MD FACP
The call was not ordinary. A grandmother was requesting help for a visiting, out-of-town family member: her 10-year-old granddaughter. She had traveled here from out of state to join a family vacation. Unfortunately, she had become ill with fever and sore throat. The grandmother was worried, both about her and about others on the trip. Dr. Kelly offered referral to a pediatrician, but she said that she would like his help, so the grandmother and the granddaughter came to the office.
The child was not particularly ill. Dr. Kelly spoke with her mother on the phone and requested a release for treatment. This was provided via e-mail. She could be treated in the office or the child could be referred to a Pediatrician's office. Well aware of her options, she requested that Dr. Kelly proceed and take care of her daughter.
A culture was obtained and treatment initiated. The culture came back: there was no Streptococcus or other pathogen. This was likely a viral illness. As there was no fever by this time, the child posed little risk to others, and the vacation went along as planned.
The grandmother called at around 9 o’clock. The patient was seen at around 10:30 and was out of the office before 11:30. As a Premium Medical Home subscriber she was able to get direct and immediate access to her physician for her family member.
This is one of the advantages of a Premium Medical Home. When a family member or a visitor from out of town needs medical help, a host always has options. Emergency rooms are open 24/7. Urgent care clinics are available. Some family medical offices have walk-in clinics. As a Premium Medical Home subscriber, you have an option: call your physician directly for help, even when the patient would be new to the doctor's practice.
BREAST CANCER SCREENING: IT’S COMPLICATED by Allan R. Kelly MD FACP
A recent study from Norway looked at the question of mammography and the over-diagnosis of breast cancer. There has long been interest in whether annual mammography poses any risk to patients.In the past, there was study and recognition of the effect of x-rays on women with annual mammography. The risk of x-ray was straightforward and the dose has been greatly reduced. More challenging is the concept of "over-diagnosis" of invasive breast cancer.
NEXIUM, PRILOSEC, AND THEIR RELATIVES by Allan R. Kelly MD FACP
As medications come into widespread use, we learn more about their risks and benefits. This does not mean a medication becomes more dangerous, but that we know better how to use it, what to look for, and we learn about rare side effects or complications.
STATIN DRUGS: WARNINGS AND REASSURANCE by Allan R. Kelly MD FACP
Statin drugs like Lipitor, Simvastatin, and Crestor are known to reduce the risk of heart attack and stroke in many groups of patients. These drugs save lives.
When initially introduced, the risk of liver disease from statins was highlighted and there was an FDA warning that all patients on statin drugs should have liver testing done. This year the FDA has removed that warning.
MEDICARE WELLNESS VISIT by Robert H. Kelly MD FACP
Beginning in 2011, Medicare has directed doctors to offer an Annual Wellness Visit (AWV) to its beneficiaries. This concept of an annual check-up applies to all health conscious persons. In the past, such a visit was often referred to as an annual physical, but that name does not well describe the goals of an Annual Wellness Visit.
NEW FEES
Two years ago we launched Premium Medical Home to expand communication and enhance the relationship between you and your doctor. In order to maintain this high level of service and communication, we are adjusting the annual subscription to Premium Medical Home. The new rates will become effective July 1, 2012 and will be reflected on your statement as you reach your anniversary date for renewal.
PMH QUOTATIONS SPRING 2012
"While the convenience of electronic storage and retrieval of medical tests is undeniable, I am concerned about the likelihood of having to pay attention to the laptop to the detriment of the patient. The foundation of medical care starts with the patient-doctor interaction. That something so fundamental be disrupted by EMR's may be one of the reasons for their slow adoption .
" - Corey Krueger, MD, FACP, 2012
"The glory in medicine is that it is constantly moving forward and there is always more to learn."
- William Mayo, MD
PMH STORY by Robert H. Kelly MD FACP
I walked into my first medical care class. For two years, I had been studying medical science. Now it was time to learn about medical care: the clinical rotations. Surgery, Medicine, Pediatrics, all the sub-specialties: I had been waiting for this day.
A respected physician was at the front of the lecture room. There were 200 eager and intelligent medical students sitting in rapt attention. This was their first clinical lecture.
The gray-haired and thoughtful physician stood before us. He began his talk, and he said that he was there to tell us what the most important job was for a physician. We students leaned further forward. Newspapers were put down. Pens stopped clicking. Conversations were hushed. Four hundred eyes and 400 ears were tuned in to what the esteemed professor was about to say.
Many of us thought that he would say that cardiopulmonary resuscitation was the most important job that we would have, bringing those who had nearly slipped from our world back into life. Others thought that perhaps it would be the delivery, not only of a single birth, but perhaps twins or triplets. Others reasonably believed that the key issue would be the public health services of vaccination and prevention. Maybe research: the discovery of the next polio vaccination. Saving life. Preventing death. We all waited, knowing that our dreams of greatness would be confirmed by what our teacher was about to say.
"The first and most important job of a physician is to identify who is sick and who is well." He let that thought sink in. The room remained silent. Clearly this could not be our most important job. It had to be something bigger. The doctor went on to explain.
Doctors are needed to identify those who are sick and who are well. If they fail to identify those who are well, then people who are not sick will be treated, subjected to examinations and procedures that are not necessary, that are associated with cost and risk. At the same time, to fail to identify those who are sick leaves those suffering without the treatment that could give them comfort. In the world today, a common belief is that our problems are caused by some illness; there is disease that accounts for what is wrong. However, that is not always the case. Often, a person is well, and the problems they experience do not arise from disease, but arise from living, the normal function of the body, and the challenges that we all face.
At the very start of helping another person as a physician, the first job, the job this professor told me about 31 years ago, is to identify who is sick and who is well. Assistance, care, treatments, advice, and counseling can follow.
CANCER SCREENING GUIDELINES by Allan R. Kelly MD FACP
The American Cancer Society is a helpful source of information about cancer and cancer screening. In our offices we use the American Cancer Society (ACS) Screening Guidelines or the United States Preventive Services Task Force (USPSTF) to help give our patients good advice. Though The American Cancer Society is reliable, it is not above criticism.
NARCOTICS OVERDOSE AND DEATH by Allan R. Kelly MD FACP
The Center for Disease Control in JAMA, December 14, 2011, reported on troubling increases in death rates from prescription pain medications.
Over the past 10 years, the sale of prescription narcotics has increased 400%.This is an extraordinary increase. But the increase is not consistent. For example, non-Hispanic whites and American Indians are three times more likely to have narcotic prescriptions than Hispanics and Blacks.
CARDIOVASCULAR DISEASE by Robert H. Kelly MD FACP
For the last 40 years, knowledge of risk factors for lifetime risk of cardiovascular disease has been accumulating. This work was first studied in a town in Massachusetts, Framingham, where the earliest evidence of risk factors was identified. There is now a Framingham Risk Calculator, for example, which uses standard risk factors to calculate the risk of heart attack and stroke.
LOWER BACK PAIN AND YOGA by Robert H. Kelly MD FACP
Back pain is common. The best approach to a strained back or common backache is to continue with usual activities and try to resume a program of non-strenuous walking. Back exercises and simple over-the-counter remedies are useful adjuncts. Extensive evaluations or dangerous treatments are usually not helpful and, if research is correct, are counterproductive.
PMH QUOTATIONS WINTER 2012
The number of medical students who choose to train for a career in primary care internal medicine has been falling for decades and has now reached a critical point. If the trend is not reversed, many patients in the US will be left without access to a primary care internist "
- Joseph S. Alpert, M.D. , Editor in Chief American Journal of Medicine, 2011
"The treatment of a disease may be entirely impersonal; the care of a patient must be completely personal."
- Francis Peabody, M.D.(1881–1927) The Care of the Patient
PMH STORY by Allan R. Kelly MD FACP
An elderly patient suffered aortic stenosis, a type of heart disease which can lead to poor heart function. Ten years earlier he had coronary artery bypass grafting on two occasions without complications and the aortic valve did not warrant repair. As the patient entered his 80's, the aortic stenosis became more of a problem: he would need surgical treatment or suffer heart failure and premature death. But in the setting of two prior heart surgeries in an 80 year old, the feasibility of aortic valve replacement seemed virtually impossible.
The patient's cardiologist referred him to a surgeon in Dallas doing a research study of percutaneous aortic valve replacement. The PMH internal medicine doctor was not part of this referral. The patient and his family asked the PMH doctor to review the protocols, talk to the doctors in Dallas and Tarrant County and share his opinions about the options. The patient benefited by talking about his problem with his PMH physician.
The PMH doctor also discussed the case with the surgeon in Dallas and made sure the surgeon had all the information he needed for enrolling the patient in the research study.
The implantation of the experimental valve went well, relieving the patient of his heart failure symptoms and resolving the problems of heart weakness. Upon leaving the hospital, the surgeon commented to the family, "Your primary doctor really cared."
Your PMH doctor is available to help you with difficult questions. Your private doctor, though no substitute for skilled sub-specialists and surgeons, is likely to have information and insight to help understand options. This direct availability and counseling is not described in CPT codes. We believe that this type of availability helps define a Premium Medical Home experience, like having a doctor in the family.
EXERCISE PROTECTS AGAINST COGNITIVE DECLINE by Allan R. Kelly MD FACP
Memory problems are common. But when do memory problems become an illness: Dementia or Alzheimer's disease? There are other reasons why memory may seem impaired………
EXERCISE PROTECTS AGAINST COGNITIVE DECLINE by Allan R. Kelly MD FACP
As reported elsewhere in PMH@ Home, cognitive decline is a common problem. We all know that memory changes as we get older, and many of us find it increasingly handy to keep a list in our pockets to help us remember………..
COUGH: OFTEN MORE BARK THAN BITE by Robert H. Kelly MD FACP
Cough is a common symptom. An acute cough is one described as lasting one to two weeks; subacute cough lasting three to eight weeks; and chronic cough more than eight weeks…………
OVARIAN CANCER SCREENING by Allan R. Kelly MD FACP
Ovarian cancer is an uncommon but often lethal form of cancer. While we have reasonable screening for cervical, colon, and breast cancers, the benefits of screening for ovarian cancer is unproven. In fact, the United States Prevention Services Task Force recommends against screening for ovarian cancer.
Medical Quotes:
"Reducing medicine to economics makes a mockery of the bond between the healer and the sick."
- Pamela and Jerome Groopman MD
"When we ourselves are ill, we want someone to care about us as people, not as paying customers, and individualize our treatment according to our values. "
- Pamela and Jerome Goodman MD
PMH STORY by Allan R. Kelly MD FACP
A Premium Medical Home subscriber was traveling to visit family. While in New York City on Saturday morning, she noticed pain and discomfort in the hip. Shortly thereafter, she noticed a rash and was uncertain of the cause, but it was both painful and visible. She called her Premium Medical Home doctor for advice.
Talking with the patient, the diagnosis was not immediately clear. The doctor knew that an examination of the rash would probably settle the diagnosis. He asked the patient to use her cell phone to take a picture of the rash and send it to him.
The picture was duly sent within two to three minutes. The photo demonstrated a rash consistent with shingles.
The doctor called the subscriber back and reviewed her symptoms and medical history again. The doctor asked her to look out the window of her hotel and see if she saw a pharmacy. There was one right across the street. The doctor called the pharmacy and ordered medication for shingles.
On returning to Fort Worth two days later, the patient had a consultation with a dermatologist, who confirmed the diagnosis that was made over the weekend. Medications were continued. Early treatment reduces the pain and suffering of shingles in mature patients. This patient got treatment quickly and conveniently.
Premium Medical Home encourages patients and doctors to work together in a way that is comfortable and convenient. We believe that this focus is not only valuable itself, but improves medical care, improves outcomes, and improves satisfaction. The patient would have received the same treatment, perhaps, in an emergency room or urgent care clinic. But ready availability of her doctor allowed for more comfortable, convenient, and timely evaluation. Such options are a benefit of your PMH subscription.
This is why we have changed our practice to the Premium Medical Home model. We believe that by focusing on the Premium Medical Home model, we can find better ways to help our patients.
ELECTRONIC HEALTH RECORDS by Allan Kelly MD FACP
There is a lot of interest in using electronic health records. Recent legislation from Washington awards doctors incentives of up to $55,000 over three to four years if they will convert their offices from paper records to an electronic record.......
PREVENTING DIABETES by Robert Kelly MD FACP
Pre-diabetes is common. It predicts a high probability that in the person's future, diabetes mellitus will develop.In the last 20 years there have been significant changes in the average American's diet and activity. One measure of this was that in about 1990 only one of the 50 states had…..
SMOKERS SUFFER by Allan Kelly MD FACP
We all know that smoking is bad for our health, but did you know that current smokers suffer poorer outcomes of other illnesses, even when those illnesses are unrelated to smoking? A smoker may philosophically accept the fact that ……
CHANGES IN DIET/LIFESTYLE AND LONG TERM WEIGHT GAIN by Robert Kelly MD FACP
A recent study from the National Institutes of Health (this is not an article on wasteful government research!) looked at food habits associated with weight change. Four items were each associated with significant weight gain…….
Medical Quotes:
"Although scientific knowledge is available to all, there is a vast difference between the best and worst of doctors, that difference representing the art of medicine."
- D. J. Weatherall, M.D., 2011
"While medicine is a science, in many particulars it cannot be exact, so baffling are the varying conditions of human life. " -
Charles Mayo, 1909
PMH STORY by Robert Kelly MD FACP
"My direct access to you and your attention to the details of my care is worth a million." A gentleman's pain had begun unexpectedly. There were questions whether or not the pain was caused by a disease which would require surgical intervention. He had undergone cervical spine surgery in the past for a painful condition and had done well, so the possibility of another surgery was considered.
After seeing the patient in the office he was admitted directly to the hospital. Over two days, he was seen by subspecialty caregivers to assess why this pain in the lower back was occurring. Unfortunately, an emergency at home prompted him to have to leave the hospital unexpectedly before definitive care.
At home, after addressing his emergency, pain, nausea and vomiting persisted. He called his PMH doctor and reported that the pain was not improving and he was having recalcitrant nausea and vomiting. He was again directly admitted to Harris Hospital for further care.
In the hospital, a team from neurosurgery, urology, and palliative medicine, including an anesthesiologist, saw the patient. After five days in the hospital with attention to pain relief he showed no need for surgical intervention, and the pain began to abate. He was able to eat, and the nausea and vomiting resolved.
The patient was pleased by the way, at each step, he had been able to reach his doctor and describe his complaints. This led to prompt effective intervention. His quote appears above.
Subscribing to Premium Medical Home and being a patient in a Premium Medical Home benefits subscribers and patients. It allows direct access. It provides attention to interdisciplinary care and the attention, when appropriate, of a subspecialty team coordinated by a trained expert physician who knows the patient well. This is a great value to patients and family.
DO STERIOIDS HELP JOINT PROBLEMS by Allan Kelly MD FACP
Common joint and tendon problems can improve with exercise and weight loss. Pain relief can be achieved with drugs like Tylenol, and elastic supports can be helpful at the wrist and the ankle and the elbow. Other interventions are less certain......
THE RISK OF BLOOD CLOTS FROM LONG FLIGHTS by Robert Kelly MD FACP
The risk of blood clots goes up after a long airplane ride, The absolute risk is low, less than 1%. In an average group of 400 passengers on a flight lasting for 12 hours, it is probable that one person may have an episode of blood clot from the flight.....
FATIGUE by Allan Kelly, MD FACP
Fatigue is a common symptom for patients making a doctor appointment. Fatigue is something that we all experience: It can be a part of our daily life, even in people who are healthy and strong. Fatigue is also a common manifestation of illness. Infection, malignancy, metabolic diseases, diabetes, and others will, in the natural history of the illness, cause fatigue........
NEW CANCER STATISTICS by Robert Kelly MD FACP
The March issue of CA, a cancer journal for physicians, included a review of cancer incidence. Worldwide, approximately one third of cancer deaths were potentially avoidable through reducing major risk factor, including tobacco use, unhealthy diet, physical inactivity, infection, unsafe sex and alchol use.........
Medical Quotes:
"Medicine, at its fundamental, is still about suffering, healing, and comforting; it is about individuals; it is about relationships and trust; it is about stories…… Concern of coding, billing, documenting, administration, computers, surveys, rules, regulations, and politics have increasingly occupied my mind and space like an intracranial tumor."
- Michael Monroe, JAMA, Volume 305, No. 12, Page 1176 to 1177
VACCINATIONS AGAINST CANCER by Allan R. Kelly MD FACP
Vaccinations have been a great gift to mankind. Some were called miracles. The development of the first vaccination for smallpox saved hundreds of millions of lives. The benefits can hardly be exaggerated, and now we see that the disease smallpox is effectively eradicated.
FULL BODY AIRPORT SCANNERS by Allan R. Kelly MD FACP
Are full body airport scanner safe? The Transportation Security Administration (TSA) uses backscatter x-ray to screen travelers. We know that many of our Premium Medical Home members will be going through airport security, and we want to let you know what we know about the new back scanner machines.
NUTRITIONAL SUPPLEMENTS: Less May Be More by Robert H. Kelly MD FACP
Nutritional supplements continue to receive a lot of attention. Shelves of stores are loaded with different supplements. Within a single class, such as vitamin D, there multiple different preparations, origins, strengths, and promised benefits.
PREVENTIVE CARE: Prostate Cancer Screening by Robert H. Kelly MD FACP
The United States Preventive Services Task Force (USPSTF), a national organization that looks at clinical effectiveness of screening and prevention methods, examined the records of nearly 400,000 asymptomatic men 45 to 80 years old. Screening with digital rectal examination and PSA was done.
Medical Quotes:
All patients are interesting, but not all doctors are interested."
- Herb Fred, M.D., Houston, Texas
"First I will define what I consider medicine to be. In general terms, it is to do away with the suffering of the sick, to lessen the violence of their diseases …"
- Hippocrates
PMH STORY by Robert H. Kelly MD FACP
A Premium Medical Home member's adult daughter became ill with fever, swollen legs and red skin. The daughter had called her doctor's answering service, but her doctor was not on call. The on call doctor did not return the daughter's phone call. The daughter was concerned and so were the parents. She was not covered by a health insurance policy.
The Premium Medical Home member called and told Dr. Kelly about their daughter's health concerns. Dr. Kelly offered to see the patient at 7:00 the next morning in the emergency room, but the family was understandably cost conscious and realized these costs could be avoided by meeting in the office. Because the Premium Medical Home office had reduced the size of the practice to a more optimal level, there was time Friday for the member's daughter to come to the office for a prompt evaluation.
Dr. Kelly saw the patient and recognized the severity of the condition: the family was right to be concerned. Urgent testing and out-patient x-ray led to the diagnosis. Treatment was effective and the patient learned how this problem might be avoided in the future.
As a Premium Medical Home member, members can call Dr. Kelly regarding an out of town guest or family member who needs medical care. Sometimes healthy younger people lack a physician relationship. Though there is no guarantee that Dr. Kelly will be able to see the out of town guest or family member, as a member, you can count on rapid enhanced access to an expert physician, who will consider the needs and recommend action for the problem you face. This is a real benefit, both to the Premium Medical Home member and also to the member's friend, guest, or family.
Often Dr. Kelly will be able to visit and temporarily serve as that guest's doctor. This allows a timely expert opinion in an environment preferred by the guest or family member. This is often all that's needed and is more convenient and economical than going to the emergency room.
If an out of town guest is with you and needs medical attention, or if a family member without access to a physician has trouble, then as a Premium Medical Home member you know you can call for help. We will visit on the phone and, if prudent and agreeable, then meet with the guest or family member so that their medical needs are met.
INFLUENZA: Time To Get Vaccinated by Allan R. Kelly MD FACP
"The 2009-2010 flu season is over and what an exciting one it was. For the first time in thirty years a serious pandemic H1N1 influenza virus appeared in the United States. It caused much confusion and we feared the worse......"
VITAMIN D, AN IMPORTANT PART OF HEALTH by Robert H. Kelly MD FACP
"Vitamin D is in the news. One recent journal article was titled "Vitamin D: Super Drug". Claims range from preventing multiple sclerosis, cancer, colon polyps, and dementia to strengthening bones and reducing aches & pains......."
NOCTURIA (NIGHTTIME TRIPS TO THE BATHROOM) IMPROVES WITH LIFESTYLE CHANGE by Allan R. Kelly MD FACP
"Waking up at night to go to the bathroom is a common adult experience. This problem is called nocturia. For many adults nighttime voiding increases as time goes by. Nocturia can be a sign of illness, such as prostatism or more serious illness, such as infection or cancer......"
Medical Quotes:
The patient should be managed the way the doctor or a member of his family would wish to be treated if he were the patient in the bed at that time."
- Robert F. Loeb, MD
"There are individuals – doctors and nurses, for example – whose very existence is a constant reminder of our frailties; and considering the notoriously irritating character of such people, I often wonder that the world deals so gently with them."
- Osler, MD
A PMH STORY – DIRECT CONTACT YIELDS DIRECT RESULTS by Robert Kelly MD FACP
An elderly woman was discharged from the hospital after a difficult illness and transferred to a long-term care facility or nursing center. She and her husband were early subscribers to the Premium Medical Home.
It was not a long term care facility that Dr. Kelly visits so she was assigned to the care of the facility medical director. The patient and her husband preferred this facility because it was more convenient for him to visits.
After she was discharged from the hospital in the afternoon, her husband accompanied her to the nursing center. When he left he saw the security system at the front door. He did not understand how it worked, but saw it would be locked in the evening. When he left for home that evening, her medicines had not yet arrived. Arriving home, finishing supper, he tried to call the facility to see if she had been given her evening medicines.
After calling many times, he realized no one was answering the phone. Alarmed, he called Dr. Kelly on his cell phone. The call was directly answered. Dr. Kelly listened to the story and recognized that the phone number the husband was dialing was not the best number to reach the nurses’ station. In a 3-way conversation, Dr. Kelly called an alternate number and got the nurse on the phone. The husband's intuition was correct – the needed medicines had not arrived and delivery was not certain.
The nurse provided the simple code for the front door lock so that the husband could come and go as he wished. Speaking with Dr. Kelly, she also agreed that if the husband were to bring the medicines from home, the nurse would see that they were promptly given to the resident and avoid any further delay or anxiety. This was a great relief to the husband and a great comfort to the wife because of her painful symptoms.
Such is the usefulness of direct contact with your PMH doctor. Knowledge and understanding about how long-term care facilities, hospitals, and other parts of healthcare systems operate was immediately available to the subscriber. This kind of enhanced access solved this problem and also relieved alarm, worry, and uncertainty. In a standard medical office, a phone call expressing concern about an inability to complete a phone call to a nursing home or getting a combination to a security door would generally not be met with direct help and intervention. At a Premium Medical Home, we are available to help with the medical needs that are important to you.
FITNESS AS PREVENTION-A SCIENTIFIC FACT by Robert Kelly MD FACP
On Sunday morning a young man wakes up and discovers a rash. What should he do? Rashes can be serious – the patient needs to see a doctor soon, but the doctor's office is closed on the weekend. The young man started a new and vital medication two weeks ago, and this could be an allergic reaction.
PREVENTION OF HEART ATTACH, STROKE AND DEATH IN DIABETICS by Allan Kelly MD FACP
"Diabetics and all adults are at risk for vascular complications. Hopefully, your doctor can help you to prevent and delay such problems….."
CANCER DEATHS DECREASING by Allan Kelly MD FACP
"Recent reports from the American Cancer Society indicate decreasing rates of cancer over the past ten years. Overall, cancer diagnoses have been declining approximately 1% per year over the 8 years and deaths have declined 1.6% per year over the past six years…"
Medical Quotes:
"It's a poor government that does not realize that the prolonged life, health and happiness of its people are its greatest asset." –
Charles Horace Mayo
PMH STORY by Allan R. Kelly MD FACP
On Sunday morning a young man wakes up and discovers a rash. What should he do? Rashes can be serious – the patient needs to see a doctor soon, but the doctor's office is closed on the weekend. The young man started a new and vital medication two weeks ago, and this could be an allergic reaction.
As a PMH Subscriber, the young man has access to his doctor 24/7, so he is able to get in touch with his doctor immediately via cell phone, even on Sunday morning. In this case, the doctor is on his way to the hospital to make rounds when he receives the call. He meets the young man at the hospital, allowing him to bypass the ER. The doctor quickly assesses the problem, determines that the rash is a reaction to the new medication, recommends care, and schedules a follow-up visit, all within an hour.
For a patient who is not a PMH Subscriber, emergency care necessitates visiting the emergency room or an urgent care clinic. These options are time-consuming, expensive, and require the patient to be treated by an unfamiliar doctor who has no prior knowledge of the patient's medical history, conditions, or medications.
For PMH Subscribers, enhanced communications options enabled the young man to see his primary care doctor without delay, eliminating hurdles and expenses. As the patient's primary care provider, the PMH doctor is familiar with the patient and can recall critical medical information from prior visits. And importantly, the follow-up visit will be with the same doctor who examined and treated the patient on Sunday.
We believe that such availability and responsiveness improves care while simultaneously reducing costs. In this scenario, the patient had a better experience at a lower cost, and he can be confident in the doctor's ongoing attention and care. We call this a Premium Medical Home experience.
RISK ASSOCIATED WITH CT SCAN FREQUENCY by Allan Kelly MD FACP
"Healthcare topics are receiving significant coverage in the media, and one issue that has received considerable public attention concerns testing and screening procedures. Medical institutions are changing their recommendations for frequency of screenings like mammography, and physicians have to balance these recommendations with what is appropriate for their patients……."
DISCUSSION ABOUT A FORT WORTH MEDICAL SCHOOL by Robert Kelly MD FACP
"The four most common cancers in the United States are cervical/prostate cancer, gastrointestinal cancer, lung cancer and breast cancer. The most common cause of cancer death is lung cancer, followed by cancer of the colon….."
CAUSES OF CANCER IN THE UNITED STATES by Robert Kelly MD FACP
"The four most common cancers in the United States are cervical/prostate cancer, gastrointestinal cancer, lung cancer and breast cancer. The most common cause of cancer death is lung cancer, followed by cancer of the colon….."
Medical Quotes:
"The practice of medicine is predominantly a humanistic act. Physicians must care about their patients, and they must constantly improve their scientific knowledge about disease. To care and not know is dangerous. To know and not care is even worse. Caring and knowing must be combined to succeed in doctoring." –
– J. Willis Hurst, MD